ORIGINAL STUDIES
BACKGROUND: In KhMAO-Yugra, every year there is an increase in the number of cases of type 1 diabetes mellitus (DM1) among residents of the district. The preservation of small indigenous peoples is an important demographic problem that requires an integrated approach. HLA-typing makes it possible to identify genetic markers of predisposition to type 1 diabetes mellitus (DM1) in the early stages of the disease and to ensure its prevention.
AIM: Identification of the frequency of carriage of polymorphic alleles and haplotypes in the loci of the HLA-DQA1, HLA-DQB1 and HLA-DRB1 genes of the HLA class II system in samples of the indigenous khanty population and the alien population permanently residing in the territory of KhMAO-Yugra.
MATERIALS AND METHODS. Low-resolution HLA typing was performed in 60 representatives of the khanty indigenous people, 54 conditionally healthy people of the alien population and 45 patients with type 1 diabetes mellitus (alien population) permanently residing in the territory of the Khanty-Mansiysk Autonomous Okrug.
RESULTS: The analysis of the frequency of occurrence of class II HLA alleles in the khanty cohort revealed statistically significant differences in the alleles DQA1*01:02/03; DQB1*02; *03:02; *05:02/04; *06:01; *06:02-8; DRB1*03; *04; *12; *13; *15; *16 in comparison with the cohort of the conditionally healthy alien population. A similar comparison of the frequencies of DQA1, DQB1, DRB1 alleles, haplotypes and their combinations between representatives of the alien population of conditionally healthy and patients with DM1 revealed significant differences in loci DQA1*01:02/03; *03:01; DQB1*06:02-8; DRB1*07, characteristic of Caucasians. When comparing the frequencies of haplotypes in Hunts with a cohort of conditionally healthy newcomers, a statistically significant low frequency of haplotypes associated with a high and moderate risk of developing DM1 (DR4~DQ8, DR3~DQ2) and a high frequency of «protective» haplotypes DQ6~DR15, DQ6~DR13 were noted.
CONCLUSION: In the khanty cohort, the frequency of occurrence of three haplotypes predisposing to the development of DM1 was reduced, and two protective haplotypes were increased, in comparison with the cohort of a conditionally healthy alien population. This determines the significant role of genetic factors in the observed low predisposition to the development of type 1 diabetes in the khanty population.
BACKGROUND: The significance of determining insulin resistance (IR) in people with type 1 diabetes mellitus (T1DM) is determined by the acceleration of the transition from the first stage of development of T1DM to the second and third, and is also a risk factor for the development of chronic complications of diabetes. The lack of a unified criterion for determining metabolically significant insulin resistance in patients with T1DM determines the need to study this problem.
AIM: To study the incidence of insulin resistance in individuals with T1DM over 18 years of age and disease duration of more than 1 year based on the estimated rate of glucose utilization and to determine the association between the eGDR value <8.77 mg/kg/min and the incidence of chronic complications of diabetes.
MATERIALS AND METHODS: 201 patients with T1DM over 18 years of age and T1DM duration of more than 1 year were examined. Among them, 95 (47%) were men, 106 (53%) were women. Median age was 30.0 [28.1; 33.0] years, median duration of T1DM — 13 [12; 15] years. The estimated rate of glucose utilization was estimated using the equation of Williams K. et al. (2000). Patients with an eGDR value <8.77 ml/kg/min were considered to have metabolically significant IR.
RESULTS: The value of eGDR <8.77 ml/kg/min (group 1) was observed in 113 (56.2%) patients. The doses of prolonged insulin both in absolute units and per kilogram of weight were significantly higher with eGDR <8.77 ml/kg/min (p=0.007 and p=0.037, respectively). Smoking, triglyceride levels, and patient age were risk factors for IR. Low insulin sensitivity was an independent risk factor for diabetic nephropathy and vascular atherosclerosis of lower extremity.
CONCLUSION: The fairly high prevalence of IR among patients with type 1 diabetes, the risk of developing diabetic nephropathy and atherosclerosis of the arteries of the lower extremities in these individuals, justifies the need to identify this condition in clinical practice in order to improve the course of type 1 diabetes.
INTRODUCTION. Therapeutic education for patients with diabetes mellitus is an integral part of their treatment. To date, in the Russian Federation, it is recommended to use distance education after completing full-time training. Following this recommendation is quite problematic due to the remoteness and lack of «Schools for patients with diabetes mellitus» in many regions of the Russian Federation. In foreign literature, the issue of distance education as an alternative to full-time is actively discussed.
PURPOSE. Highlighting the effectiveness of distance education using telemedicine technologies in patients with type 2 diabetes.
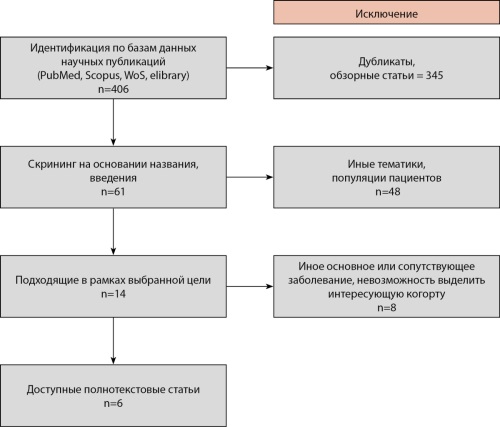
МETHODS. A systematic search was conducted for scientific publications comparing traditional forms of education with online education in patients with type 2 diabetes, according to the recommendations of PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses). Clinical studies using distance education in patients with type 2 diabetes without comparison with the full-time form were excluded.
RESULTS. In total, six scientific publications were selected, in which the distance education form was compared in parallel with traditional therapeutic education. In all studies, distance education has demonstrated its effectiveness. The small sample size, the age heterogeneity of the participants, the short-term duration of the study, as well as the different method of remote interaction and the therapeutic education program are limitations for assessing the overall effect.
CONCLUSIONS. The use of telemedicine technologies in therapeutic education in patients with type 2 diabetes offers great prospects for increasing the availability of training and improving the quality of medical care.
REVIEWS
Continuous glucose monitoring (CGM) has been established as a method for self-assessment glucose levels in individuals with diabetes mellitus in the Russian Federation for more than 15 years. The main characteristics of CGM sensors are its’ accuracy and performance that ensure their effectiveness and safety. Currently, there are no standardized guidelines that outline the minimum accuracy standards for CGM systems.
This review is aimed to codify the current methods for evaluating CGMs accuracy and performance across the different countries, as well as to propose local Russian guidelines on CGM device accuracy evaluation. This involves guidelines for the design of clinical trials to assess sensors accuracy and the minimum acceptable performance requirements for CGM devices to be utilized in clinical settings.
Psoriatic arthritis (PsA) and psoriasis (PsO) are often associated with metabolic disorders including obesity, metabolic syndrome, diabetes mellitus (DM) and cardiovascular diseases (CVD). It is believed that obesity, DM, PsO and PsA have similar immunopathogenetic mechanisms. Chronic inflammation is closely associated not only with the development of PsO and PsA, but also with the formation of insulin resistance and the development of DM. In patients with DM, as well as with PsO and PsA, acute phase indices and proinflammatory cytokines are increased, including C-reactive protein, tumor necrosis factor α (TNF-α), interleukins 1 and 6 (IL-1 and IL-6), which, regardless of the presence of obesity, are associated with the development of insulin resistance. In PsA and PsO, the use of TNF-α inhibitors increases insulin sensitivity and reduces insulin resistance. It has been shown that the IL-12/23 inhibitor Ustekinumab slows down the development of type 1 diabetes in patients with PsO. Given the high prevalence of diabetes in PsA and PsO, screening should be performed to detect the disease. When choosing therapy for patients with PsA, PsO in combination with type 2 diabetes, the ability of some drugs to improve carbohydrate metabolism should be taken into account, as well as the use of hypoglycemic drugs if necessary.
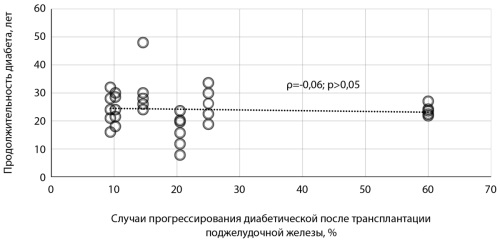
The effect of pancreatic transplantation on the condition of target organs in diabetes mellitus (DM) is an area that requires further study. In this literature review, studies reflecting the ophthalmological status of patients before and after pancreatic transplantation were analyzed, as well as an assessment of potential risk factors associated with the progression of diabetic retinopathy and the development of diabetic macular edema in the post-transplant period. Based on the results of the studies studied, the following predictors of the progression of diabetic fundus damage after pancreatic transplantation were identified: early age at the time of DM manifestation, absence or presence of a non-proliferative stage of diabetic retinopathy before surgical treatment of DM, panretinal laser coagulation for 1 year before transplantation, isolated pancreatic transplantation as a method of choice of transplantation, high baseline and postoperative levels of glycated hemoglobin (before transplantation — ≥9.0±2.3%, after surgery — ≥6.0±0.6%), as well as its marked decrease after surgical treatment of diabetes, arterial hypotension in the first 3 months after transplantation, arterial hypertension in the late post-transplant period. Knowledge of these risk factors can help an ophthalmologist in predicting the course of diabetic fundus changes, carrying out prevention, as well as in providing timely qualified assistance in case of deterioration of the ophthalmological status of pancreatic transplant recipients.
INTRODUCTION. One of the serious complications of diabetes is diabetic retinopathy, which is the leading cause of blindness and disability. Digital screening for diabetic retinopathy is one of the effective measures recommended by the WHO. To implement an effective digital screening program for DR, several important conditions must be met. At the same time, the organization of the disease screening at the regional level requires a comprehensive approach, which includes compliance with the recommended international experience, taking into account the characteristics of the subject. This work is devoted to determining the key steps for the implementation and adaptation of such a digital infrastructure in the Tomsk region.
MATERIALS AND METHODS: the data of the federal statistical observation form No. 12, the Federal State Statistics Service https://rosstat.gov.ru/, Tomskstat https://70.rosstat.gov.ru/. Statistical analysis methods: descriptive statistics method, time series analysis. Data processing was carried out using the «MS Office Excel 2010» spreadsheets and the «Statistica» software package for Windows 10.0.
RESULTS. The key element of the digital screening system for diabetic retinopathy in the subject was the organization of the Retinal Pathology Center, the main goal of which is the prevention of blindness and severe visual impairments in the subject. The second important condition was the development and implementation of a telemedicine system with an embedded decision support system, which united the Retinal Pathology Center and medical institutions of the Tomsk region into a single digital circuit. The third condition was the adaptation of the routing of patients with retinopathy into the existing routing scheme for patients in the «ophthalmology» profile. Another condition was the implementation of a pilot project to adapt the digital structure to the existing scheme of medical care organization in the «ophthalmology» profile in the region, the identification of first-line medical organizations, and the establishment of digital communication. The final condition was the introduction of changes at the legislative level.
CONCLUSION. The fulfillment of the above conditions allowed the successful implementation of the digital project in the Tomsk region and the creation of an organizational infrastructure for the early detection and timely treatment of patients with diabetic retinopathy.
Type 2 diabetes (T2D) is a leading cause of chronic kidney disease (CKD). This review analyzes the results of studies assessing the prevalence, clinical phenotypes, and outcomes of CKD in T2D. Over the past 20–30 years, there has been a global trend toward an increase in the number of patients with T2D and CKD. At the same time, the prevalence of CKD among patients with T2D appears to remain stable and averages 25–30%. Studies from different countries demonstrate both upward and downward trends in the prevalence of CKD among patients with T2D. This can be explained by differences in study design, CKD screening quality, and real differences in the prevalence of CKD in different populations. In patients with T2D, CKD is heterogeneous in morphological and clinical characteristics, course, and outcomes. An obvious current trend in the epidemiology of CKD in patients with T2D is an increasing prevalence of renal function decline in the absence of albuminuria. Female sex, older age, optimal glycemic and hypertension control, use of renin-angiotensin system blockers, and the absence of diabetic retinopathy are associated with non-albuminuric CKD in T2D. Patients with T2D with the albuminuric phenotype of CKD appear to have a higher risk of developing end-stage renal disease and major adverse cardiovascular events compared with patients with T2D and non-albuminuric CKD. The reported incidence of end-stage renal disease in patients with T2D varies widely, from 0.41 to 6.9 cases per 1000 patient-years. The diversity of data may be explained by differences in baseline patient characteristics and different durations of follow-up. The heterogeneity of the design of studies conducted to date, the small number of prospective studies on large patient samples make it difficult to objectively assess the dynamics of CKD prevalence and incidence in patients with T2D. Further real-world evidence studies are urgently needed to assess the epidemiology of CKD in patients with T2D.
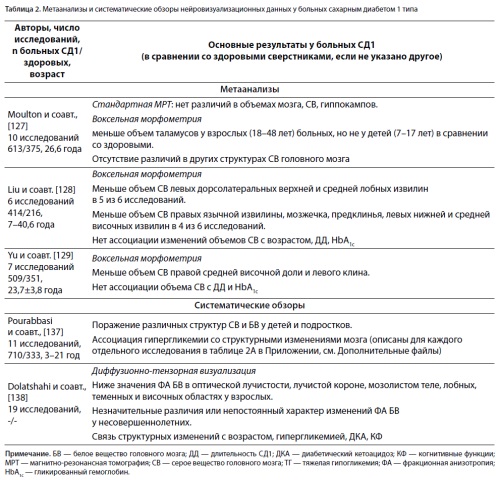
Psychoorganic syndrome (POS), also known as organic brain syndrome, or encephalopathy, is characterized by cognitive decline, emotional incontinence (emotional lability), and asthenic symptoms. It can develop due to a number of exogenous and endogenous factors, and despite the use of the term «diabetic encephalopathy», the evidence for a specific diabetic etiology of POS remains limited. The review provides a detailed history of the term POS and its definition, components and possible causes, pros and cons of the existence of POS of diabetic origin. The potential influence of dysglycemia on the development of POS and brain abnormalities in Type 1 diabetic patients (T1D) found at neuroimaging, as well as their associations between each other and with other clinical parameters, including the age at diabetes manifestation, disease duration, acute diabetic complications, and diabetic retinopathy as a marker of a long-term exposure to hyperglycemia, are discussed. In young adults with T1DM, cognitive function parameters fall within the age-related reference ranges, and their associations with the degree of hyperglycemia or severe hypoglycemia are not reproducible in larger samples. The analysis of neuroimaging and histological data also does not provide convincing evidence that brain abnormalities are unique to T1DM. Thus, the issue of POS (encephalopathy) in T1DM remains insufficiently studied and controversial. Current data does not allow to unequivocally accept the specific diabetic nature of POS/encephalopathy in T1D. Further studies are necessary to identify the contribution of diabetes and associated factors to the development of POS, including histological data.
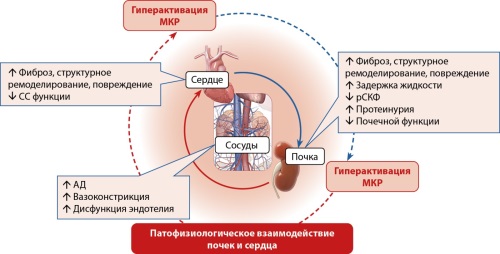
Type 2 diabetes mellitus (T2DM) is associated with hyperactivity of the renin-angiotensin-aldosterone system (RAAS), leading to increased aldosterone levels in the blood. This can result in the development and progression of chronic kidney disease (CKD) and congestive heart failure (CHF). High aldosterone levels, in turn, contribute to insulin resistance, microcirculatory disorders, mitochondrial dysfunction, oxidative stress, inflammation, dyslipidemia, and fibrosis. Additionally, in T2DM patients, persistent oxidative stress and hyperglycemia can trigger pathological activation of mineralocorticoid receptors, even in the absence of aldosterone or cortisol. This results in a vicious cycle of inflammation and fibrosis in the heart and kidneys.
Therefore, targeting mineralocorticoid receptor (MCR) blockade is crucial for reducing fibrosis and other irreversible changes in CKD and CHF, as it can help break this cycle and reduce inflammation and fibrosis. However, spironolactone is not a highly selective MKR antagonist, which is one of the reasons for its many side effects. Eplerenone, with greater selectivity and lower affinity for the MKR, has a weaker cardioprotective effect due to its lower affinity. Finerenone, a first-in-class nonsteroidal mineralocorticoid receptor antagonist indicated for the treatment of CKD with albuminuria in adult patients with T2DM, provides the most significant anti-inflammatory and antifibrotic effects without the side effects associated with steroidal anti-inflammatory medications.
The aim of this review is to evaluate the clinical trial results on the effects of finerenone on cardiovascular and renal outcomes in patients with T2DM. The review provides an up-to-date overview of the current literature on the impact of finerenone on these outcomes and systematically summarizes and describes additional positive cardioprotective benefits associated with its use.
CASE REPORTS
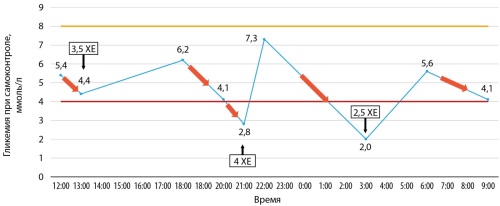
Insulinoma is a rare neuroendocrine tumor occurring from beta-cells of the pancreas. Тhe diagnosis of insulinoma may be difficult, especially in patients with concomitant diabetes mellitus. The reason for the similar clinical picture in these patients could be an incorrect scheme of hypoglycemic therapy. There is a number of cases of insulinoma in patients with type 2 diabetes mellitus described in literature. A more paradoxical clinical situation is the development of insulinoma in a patient with type 1 diabetes mellitus (T1DM). Analyzing a huge amount of literature sources, only three articles describing insulinoma in patients with T1DM were discovered. In all the described cases, the tumors turned out to be malignant. We present the first described in literature clinical case of the diagnosis and treatment of insulinoma in a patient with latent autoimmune diabetes in adults (LADA-diabetes), as well as the review of the literature on this topic. A gradual decrease in the need for exogenous insulin in combination with recurrent hypoglycemia made it possible to suspect the diagnosis, which was confirmed during a fasting test and instrumental examination of the tumor using computer tomography and endoscopic ultrasound.
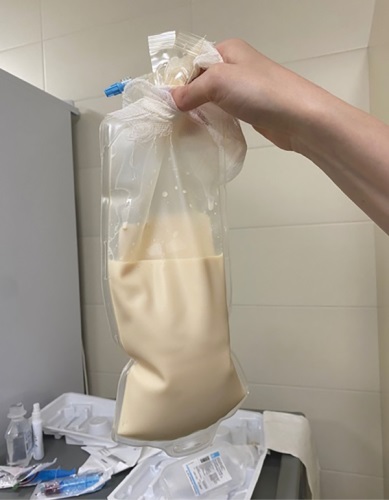
Lipodystrophies are a group of orphan diseases (according to different sources, the prevalence of the disease varies from 1 to 5 cases per 1,000,000 population), which can be either hereditary or acquired. Diseases of this group represent a symptom complex characterized by varying degrees of loss of adipose tissue: complete (generalized lipodystrophy) or partial (partial lipodystrophy), as well as abnormal distribution of subcutaneous fat, provided that there is no influence of alimentary factors and catabolic conditions. Lipodystrophies are characterized by metabolic changes: dyslipidemia, carbohydrate metabolism disorders, insulin resistance, metabolically associated fatty liver disease. Separately, it is worth mentioning reproductive disorders, such as polycystic ovary syndrome, infertility, miscarriage, and others. A decrease in the body’s fat content leads to a decrease in the production of the hormone leptin, which affects the hypothalamic neurons that regulate hunger and satiety, and increases energy expenditure by stimulating thermogenesis. Hypoleptinemia is the main cause of metabolic disorders associated with lipodystrophy. Currently, a recombinant analogue of human leptin has been registered — metreleptin (methionyl leptin), which improves the quality of life of patients by achieving compensation for metabolic disorders, reducing hyperphagia, and also having a beneficial effect on fertility.
HNF1A-MODY is diabetes mellitus with an autosomal dominant type of inheritance associated with heterozygous variants of the HNF1A gene, which is involved in the differentiation and functioning of the pancreas. The disease is characterized by onset at a young age, prevalence of postprandial hyperglycemia, presence of glucosuria, progressive course with a high risk of developing micro- and macrovascular complications, effectiveness of therapy with sulfonylurea drugs with the emergence of the need for insulin therapy over time.
This article presents the first clinical case in Russia demonstrating the pregnancy of a patient with a combination of two orphan diseases: familial partial lipodystrophy type 4 and MODY 3 (list of rare (orphan) diseases of the Ministry of Health of Russia, dated February 6, 2023), who received pathogenetic treatment with metreleptin before confirmation of the fact of pregnancy.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2072-0378 (Online)