Original Studies
Despite significant progress in the treatment of T1DM in children, achieving target levels of carbohydrate metabolism in children remains one of the most difficult tasks. The influence of the psychosocial state of the family on the ability to achieve metabolic compensation is becoming increasingly clear. However, the study of social risk factors in families with children with T1DM and their impact on metabolic control remains clearly insufficient.
The purpose of the study is to determine social risk factors (SR) that are most typical for families of children with type 1 diabetes mellitus (T1DM) in our country and to analyze their relationship with compensation for T1DM based on a survey of parents.
MATERIALS AND METHODS: The study was conducted in endocrinology departments of children’s hospitals and departments of medical and social care of children’s clinics in 4 regions - Vologda, Tyumen, Chelyabinsk regions and Khanty-Mansi Autonomous Okrug.
A total of 325 respondents took part in the study. 1 group — experience of T1DM in children >1 year and poor metabolic control (level of glycated hemoglobin ((HbA1c) >7.5%) — 195 hours; 2 gr. — experience of T1DM in children >1 year and good metabolic control (HbA1c <7.5%) — 60 people. An additional group consisted of 73 patients with <1 year of experience of T1DM in children, regardless of metabolic control, in order to analyze the prevalence of social risk factors already in the 1st year of diabetes.
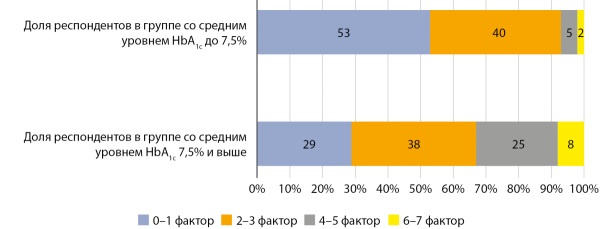
RESULTS: In the overall group, HbA1c was 9.1% (4.9–17%). The five most common SR factors were a low level of parental education (lack of higher or secondary education), lack of a permanent job, raising a child alone, lack of support from loved ones, and income below the subsistence level.
1 group (192 people). Average HbA1c level 9.8% (7.5–17%). Among the HR factors that significantly influence HbA1c levels, the level of education of parents, single parenting of a child, low family income and the number of children in the family were identified. The number of influencing social risk factors also has a negative impact on metabolic control.
2nd group. (60 people). HbA1с — 6.6% (5.3%–7.3%). The prevalence of SR factors was significantly lower than in the previous group. The differences were significant for lack of higher education, single parenting, and low family income.
3 gr. (73 people). HbA1c — 9.3% (4.9–15.1%, which may be due to the duration of diabetes less than 3 months in some children. After 3 months, the HbA1c level was 7.9% (4.8–13.4%). The list of SR factors practically coincides in composition and frequency with those in families of group 1. Thus, social difficulties that are not resolved in a timely manner aggravate the situation of the family and negatively affect the compensation of carbohydrate metabolism.
CONCLUSION. We have identified the most significant factors of SR in families with children with T1DM in the Russian Federation. The deterioration of social conditions in the family is a factor that negatively affects the level of control of T1DM and the development of complications in the future. As a result, families with children with T1DM, especially with chronic decompensation, need assessment of SD factors and support from social services.
BACKGROUND. Skeletal muscles play a key role in the organism’s carbohydrate metabolism. Dysregulation of insulin-dependent glucose uptake in skeletal muscle disrupts carbohydrate metabolism in the organism and can lead to the development of obesity and type 2 diabetes.
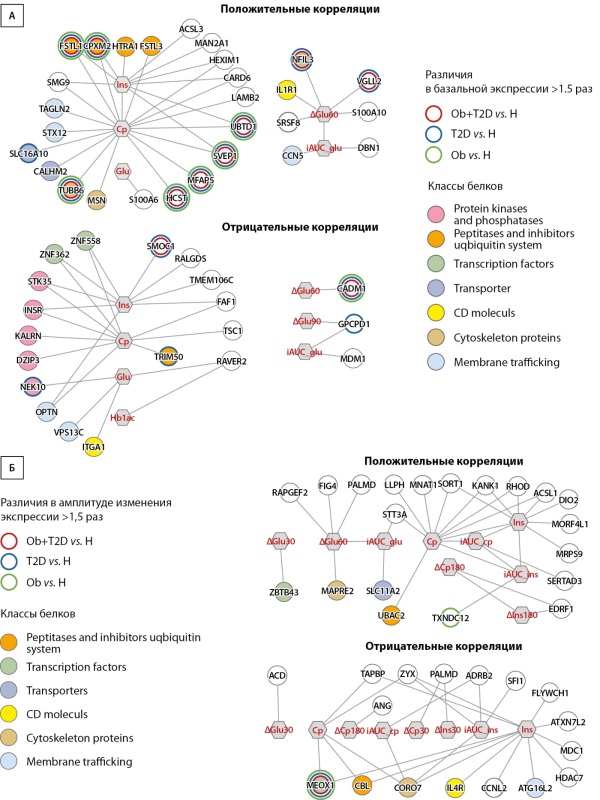
AIM. To identify expression markers (genes) of human skeletal muscle associated with disorders of glucose metabolism in the basal state and after a mixed meal normalized for body mass.
MATERIALS AND METHODS. The study involved three groups of 8 people: healthy volunteers, obese patients without and with type 2 diabetes. Venous blood samples were taken in the morning (09:00) after an overnight fast and 30 min, 60 min, 90 min, 120 min, and 180 min after ingestion of a mixed meal normalized by body mass (6 kcal/kg). Biopsy samples from m. vastus lateralis was taken before and 1 h after a meal to assess gene expression (RNA sequencing) and search for genes correlating with markers of impaired glucose metabolism in the basal and postprandial state.
RESULTS. Strong correlations (|ρ|>0.7 and p<0.001) between the gene expression and the level of insulin, C-peptide, glucose or glycated hemoglobin in the basal and/or postprandial state was found for 75 genes. Of these, 17 genes had marked differences (>1.5-fold) in expression between healthy people and patients, or differences in expression changes in response to a meal. We can note genes whose role in impaired glucose metabolism has already been shown earlier (FSTL1, SMOC1, GPCPD1), as well as a number of other genes that are promising for further study of the mechanisms of insulin resistance in skeletal muscle.
CONCLUSION. Skeletal muscle expression markers were identified as promising candidates for future targeted studies aimed at studying the mechanisms of insulin resistance and searching for potential therapeutic targets.
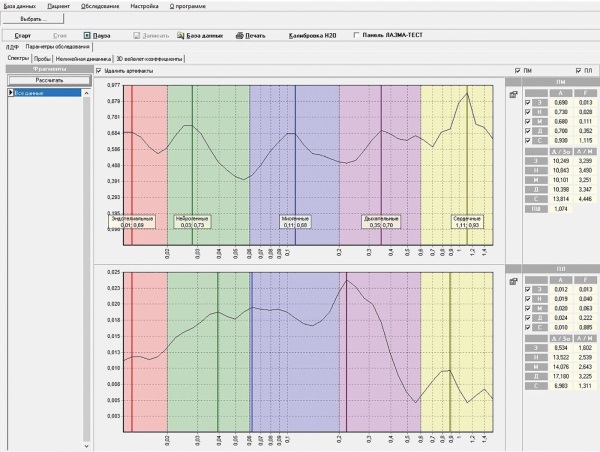
BACKGROUND: Microcirculatory dysfunction in patients with diabetes mellitus leads to tissue trophic insufficiency, reduction of adaptation reserves. It is possible to perform lifetime assessment of structural and functional changes in the microcirculation system by laser Doppler flowmetry. The presence of microcirculatory disorders is established in eyelids in chronic blepharitis and meibomian gland dysfunction. The article presents the results of the study concerning the peculiarities of neoangiogenesis as a mechanism of development of chronic blepharitis and meibomian gland dysfunction in diabetes mellitus (DM).
AIM: to reveal the peculiarities of microcirculatory disorders of the eyelid in chronic mixed blepharitis in patients with type 2 diabetes mellitus (T2DM).
MATERIALS AND METHODS: The study was conducted in 57 patients: 37 patients with chronic mixed bilateral blepharitis and a verified diagnosis of T2DM (group 1, n=74 eyes, average age 69.5 ± 7.5 years; subgroup 1a, n=38 eyes — patients with T2DM and glycated hemoglobin average level (HbA1с) 6.7±1.2; subgroup 1b, n=36 eyes — patients with T2DM and HbA1с average level 8.2±1.3) and 20 patients with chronic mixed bilateral blepharitis without signs of DM (group 2, n=40 eyes, mean age 67.2±4.3 years). Laser Doppler flowmetry was performed on the device «LAZMA MC-1».
RESULTS: In patients with chronic blepharitis against the background of T2DM the development of ischemia of the eyelid tissue with increasing tension of functioning of the regulatory systems of microcirculation blood flow and lymph flow was detected, and in persons without DM — venous stasis with moderate inhibition of vasomotor, respiratory and dominance of cardiac oscillations of blood flow, as well as insufficiency of neurogenic oscillations of lymph flow. In this case in 1a subgroup the dominance of neurogenic oscillations of blood flow was revealed, in 1b - myogenic. Microcirculatory changes of lymph flow in the 1b subgroup were more pronounced in comparison with the 1a subgroup.
CONCLUSION: The results proves the negative influence of T2DM on the microcirculatory bed of patients with chronic mixed blepharitis. The disorders detected by laser Doppler flowmetry vary depending on the HbA1с.
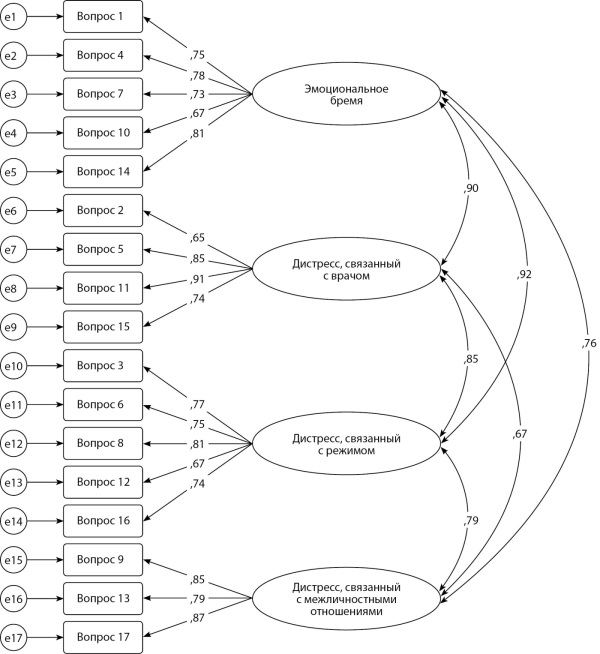
BACKGROUND: Diabetes distress (DD) is the negative emotional or affective experience resulting from living with diabetes. DD is a negative predictor of blood glucose control and quality of life, and may lead to decreased adherence to treatment. To diagnose DD, questionnaires are used to screen the emotional state and psychosocial aspects. In the study, linguistic, cultural adaptation and assessment of the psychometric properties of the Russian version of the questionnaire “The Diabetes Distress Scale” were conducted among patients suffering from T1DM and T2DM.
Patients with diabetes mellitus (DM) have diabetic distress as one of the most common mental disorders along with depression. Depression and diabetic distress increase the risk of death in diabetes, negatively affect treatment adherence and self-monitoring of glycemia. Identification of these conditions among patients with T1DM and T2DM can contribute to their timely correction.
AIM: To carry out linguistic and cultural adaptation of the questionnaire “The Diabetes Distress Scale” and evaluate the psychometric properties of the Russian version of the DDS questionnaire on a Russian-speaking sample of patients with T1DM and T2DM.
MATERIALS AND METHODS: A study was conducted on a sample of 198 patients with T1DM and T2DM; data was collected on the use of the Russian version was collected DDS scales, as well as the EQ-5D-5L (European Quality of Life Questionnaire), SPANE (Positive and Negative Experiences Scale) and HADS (Hospital Anxiety and Depression Scale) scales. The last three scales were used to assess the convergent validity of the adapted questionnaire. Reliability of the DDS questionnaire was assessed using Cronbach’s α coefficient of internal consistency and participant retest after 1–4 months.
RESULTS: The factor structure of The Diabetes Distress Scale questionnaire is fully reproduced when all 17 questions are included (measurement model fit indicators: CFI=0.981, RMSEA=0.055, TLI=0.967). The internal consistency of the subscales (α ϵ [0.836; 0.874]) and the questionnaire as a whole (α=0.948) is assessed as high. Significant correlations of the adapted methodology and its subscales with the scales of the EQ-5D-5L, SPANE, HADS questionnaires were obtained, the closest connections (Rho ϵ [0.370; 0.437], p<0.01), which indicates good external validity of the adapted methodology.
CONCLUSION: The Russian version of the DDS questionnaire has good psychometric properties. It is a valid and reliable tool for assessing diabetes distress among patients with T1DM and T2DM and can be recommended for use in clinical practice for timely diagnosing depression and DD.
BACKGROUND: Since the emergence of coronavirus infection in clinical practice, particular attention has been paid to its acute phase. However, to date, the direct and indirect impact on patients with type 2 diabetes mellitus after recovery from coronavirus infection remains an open question.
OBJECTIVE: To determine the clinical and laboratory features of the post-COVID period in patients with type 2 diabetes mellitus during different phases of the infection.
MATERIALS AND METHODS: A descriptive retrospective study was conducted using the electronic medical records of 134 patients who had recovered from coronavirus infection.
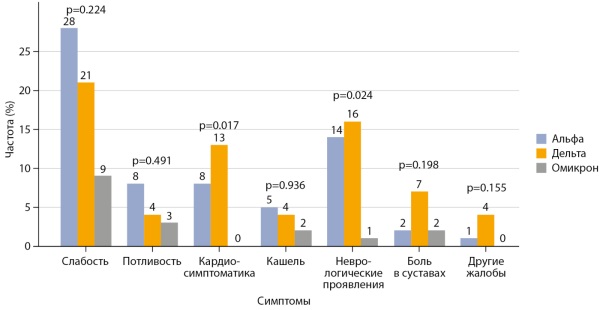
RESULTS: The majority of the patients were women, with no significant differences in age and gender distribution across the groups (p=0.384 and p=0.207, respectively). During the «Omicron» period, there were fewer comorbidities and fewer hospitalized patients compared to the other groups (p<0.0167). Regarding diabetes-related conditions, frequent urination was observed only in patients during the «Alpha» period, while the frequency of hypoglycemia, hyperglycemia, the severity of chronic kidney disease, and manifestations of polyneuropathy did not differ significantly between the groups (p>0.0167). When examining newly diagnosed diseases, a statistically significant difference was found only in musculoskeletal disorders (16.7% in «Alpha» vs. 30.2% in «Delta» vs. 3.7% in «Omicron», p=0.015). In the analysis of laboratory indicators, a difference was detected in platelet counts and activated partial thromboplastin time (APTT): median platelet counts were significantly lower in the «Alpha» and «Delta» groups compared to the «Omicron» group (210 [179.2–249.7] x10⁹/L and 218 [196.5–281] x10⁹/L vs. 255 [208–327] x10⁹/L, respectively, p=0.016). The APTT was significantly longer for «Alpha» and «Delta» compared to «Omicron» (28 [23.6–31.3] seconds vs. 30.3 [26.1–34.9] seconds vs. 27.1 [22.4–30.3] seconds, respectively, p=0.013).
CONCLUSION: Real-world data allow tracking the development of new symptoms and diseases in patients during the post-COVID period. Patients with type 2 diabetes mellitus during the «Omicron» variant-associated period had a lower risk of developing new symptoms and diseases. It is necessary to implement solutions for monitoring target HbA1c levels through medical information systems and to enhance reporting standards for patient symptoms to enable more accurate analysis Real world data (RWD).
BACKGROUND: Bariatric surgery has proven effective as a treatment for the metabolic complications of obesity, including type 2 diabetes mellitus (T2DM). Nowadays it is important to develop a personalized approach for bariatric patients generally, and for those with T2DM.
AIM: Development of a scale for preoperative prediction of remission of T2DM in obese patients Russian population undergoing bariatric surgery (sleeve gastrectomy or gastric bypass).
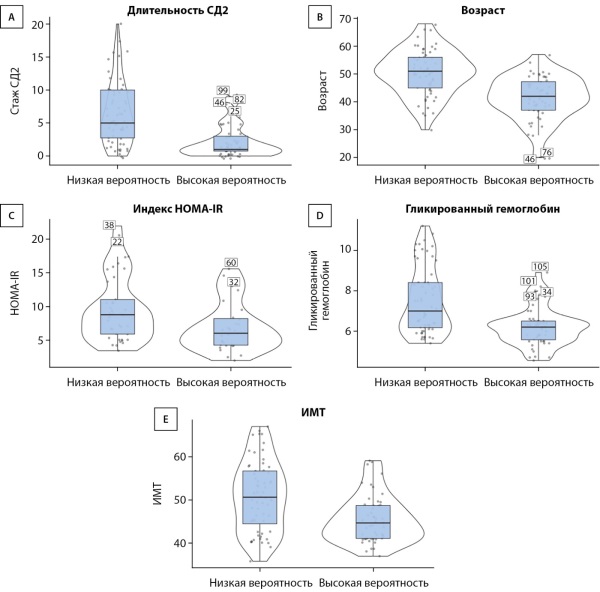
MATERIALS AND METHODS: A retrospective multicenter cohort study was conducted. The study included 112 patients (75 women and 37 men), mean age 46.25±9.29 years, mean BMI 48.71±7.66 kg/m2. A mathematical analysis of 17 preoperative clinical criteria was carried out to search for independent predictors of T2DM remission.
RESULTS: A remission of T2DM was verified in 85 subjects, (75.9%), absence of remission of T2DM — in 27 subjects (24.1%). The most important prognostic factors were T2DM experience, age, HOMA-IR insulin resistance index, HbA1c, BMI, metformin therapy, SUs, insulin intake, increased levels of liver transaminases, and total cholesterol levels. The relative importance coefficient of each parameter was calculated. A formula has been developed to predict the high or low probability of T2DM remission after bariatric treatment. An online DRAMS (Diabetes Remission After Metabolic Surgery) calculator was proposed based on this formula so it is easy to use in clinical practice.
CONCLUSION: An online calculator has been developed to predict the probability of T2DM remission after bariatric surgery. The received data allow us to construct a qualitative “high risk”/“low risk” scale. A number of identified predictors require further study in larger samples of patients.
BACKGROUND: continuous subcutaneous insulin infusion (CSII) and continuous glucose monitoring (CGM) improve daily life for people with Type 1 Diabetes Mellitus dramatically (T1D). However, there are still no compelling evidences that the use of insulin pumps (IP) and continuous glucose monitors (CGM) really help to improve diabetes control in children and adolescents.
AIM: to analyze the relation between diabetes control and the use of insulin pumps and continuous glucose monitors in children.
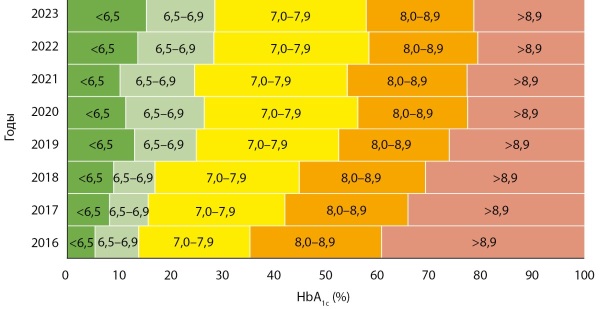
MATERIALS AND METHODS: 6382 children with T1D aged 1–18 years were enrolled in this study. Frequency of CSII and CGM use, HbA1с level and the percentage of children with HbA1с< 7.0% were analyzed.
RESULTS: HbA1c decreased from 8.6% to 7.7% for 7 years (p<0.001). Simultaneously the quantity of children with HbA1c<7.0% increased from 11% to 29%. During this period the use of CGM increases dramatically from 11.6% to 84%. The use of IP increases from 38.7% to 42.3% (p<0.001).
CONCLUSION: CSII and continuous glucose monitors use statistically significant improves T1D control in children according to mean HbA1c level decrease and the quantity of children with target HbA1c level increase.
AIM: To evaluate the impact a fixed-ratio combination of insulin glargine(100U/ml) and lixisenatide(iGlarLixi) on the glycemic control in Russian study T2D population uncontrolled on OAD ± insulin therapy in real-world settings.
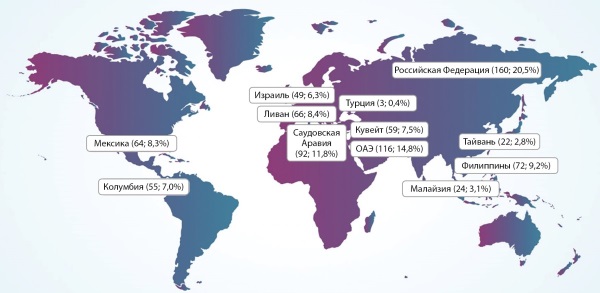
MATERIALS AND METHODS: The Russian subanalysis of international, multicentre, prospective, observational SUCCESS study included 160 T2DM patients who had initiated iGlarLixi within 1 month prior to study inclusion from 11 regions of the Russian Federation. The primary endpoint — HbA1c change from baseline to month 6. Secondary endpoints: HbA1c change after 12 months, achievement of target HbA1c levels after 6 and 12 months; change in FPG and PPG, change in body weight after 6 and 12 months, iGlarLixi dose dynamics. Safety endpoints: adverse events, serious adverse events, adverse events of special interest, frequency of hypoglycemia during the study period.
RESULTS: The average age of patients in the Russian population was 60.8±9.4 years; average duration of T2DM was 11.4 years, mean HbA1c — 9.3±1.5%; mean BMI 33.3 kg/m2. Prior to the study, most patients were on 2 (36.3%) and 3 OADs (27.5%), 32.5% — on insulin therapy. The mean change of HbA1c at month 6 was -1.81%, and -2.03% at month 12. 51.3% patients achieved individual HbA1c targets at month 12, 46.7% of patients achieved the HbA1c target without hypoglycemia and weight gain. The decrease of body weight in 12 months was -3.3±4.4 kg. During the study period, 17 cases of hypoglycemia were recorded (0.11 events per patient-year); 1 severe hypoglycemia (0.01 events per patient-year). The total number of adverse events (AEs) was 43(26.9%), serious AEs - 10 (6.3%).
CONCLUSION: According to the results of this prospective real world sub-group analysis, initiation of iGlarLixi in Russian adults with T2DM uncontrolled on OADs ± insulin significantly improves glycemic control with low risk of hypoglycemia and no body weight increase.
BACKGROUND: The primary cause of blindness in diabetics is diabetic retinopathy (DR), the most common microvascular complication of diabetes, and visual impairment. Visfatin is an adipocytokine that aids in insulin activity during gestational diabetes and pregnancy.
AIM: This study aimed to estimate serum visfatin levels in DR, proliferative (PDR), non-proliferative (NPDR), and healthy subjects (HS).
MATERIALS AND METHODS: A 120-patient case-control study with a history of T2DM for more than 5 years as well as 30 healthy subjects enrolled in the study. Patients group divided into three sub-groups, DM, PDR, and NPDR. Visfatin levels were measured using a commercially available enzyme-linked immunosorbent assay kit. Triglyceride (TG), serum cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) levels and glycated haemoglobin (HbA1c) were assessed.
RESULTS: The PDR patients and patients with poor glycemic control showed significantly increased visfatin levels compared with the HS group and T2DM patients without DR. The TC, TG, and DR group’s LDL-C levels were noticeably higher and significantly greater in PDR than in the group of HS.
CONCLUSION: Visfatin levels have been linked to both the severity and existence of DR. and more in patients with poor glycemic control. Elevated lipids were associated with DR risk.
Review
Retinopathy of prematurity (ROP) is a complex and unresolved problem in pediatric ophthalmology, leading to visual disability. Low birth weight and prematurity are the main risk factors, and they form the basis of clinical recommendations for screening for ROP in all children under 35 weeks of gestational age and weighing less than 2000 g. However, many researchers point to other risk factors that can be divided into maternal, prenatal and perinatal. In this review, we consider maternal diabetes mellitus as a risk factor for ROP. Changes in the retina in premature infants and mothers with diabetes mellitus have some common features, since pathological angiogenesis occurs at the basis of these diseases. In addition, diabetes is a risk factor for preterm birth, and prematurity is a leading cause of neonatal morbidity, including the development of ROP. This suggests that maternal diabetes mellitus may have both direct and indirect effects on the development of ROP. To develop predictive models, an understanding of risk factors for ROP, the pathophysiology of retinal vascular diseases, and diseases of prematurity is necessary.
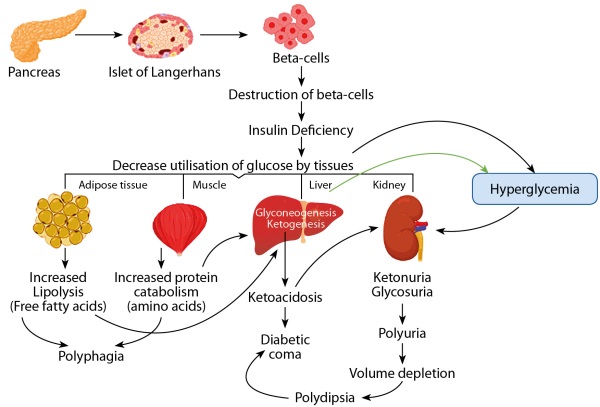
Diabetes mellitus is a chronic metabolic disorder which is commonly found life-threatening disease and it continuously reducing the life expectancy. It is characterized by hyperglycaemia (raised blood sugar level) resulting from defects in insulin secretion, action, or both. Since thousands of years, medicinal plants are being used by our ancestors for the prevention, treatment or even cure the diabetes mellitus. Utilization of these herbal plants is increasing rapidly last two to three decades due to their lesser toxicity and cost effectiveness property as compared to synthetic drugs. In this review, approximately 30 medicinal plants were described which are native to India and traditionally used by the people living in shivalik range of Himalaya in Uttarakhand (specially Dehradun & Haridwar) for the treatment of diabetes mellitus. The data about these plants was collected from science direct, PubMed, web of science, scopus, mdpi, google scholar and different other search engines and websites. This review was conferred in a systematic way as it includes botanical name, family, vernacular name, parts used and pharmacological uses of plants in a tabulated form. There are various scientific evidences behind the uses of some medicinal plants which have been mentioned along with the summary of individual medicinal plant. In this review, all the plants and herbs are easily available in these regions of Uttarakhand and local people traditionally uses these plants as vegetable, seasoning, flavouring and usually consume as a part of their diet. There are some limitations of phytotherapy which limit it to completely replace the allopathic therapy as less bioavailability, less rate of absorption and slow rate of dissolution. But by using various advanced dosage forms (phytosomes, neosomes, liposomes, nanoparticles, nanobubbles, nano diamonds, nanosphere etc.) and method of delivery (various invasive and non-invasive methods) which can bypass these all problems associated with the potency and efficacy of phytochemicals.
Case report
Type 1 diabetes mellitus (T1DM) continues to struggle with medical and social problems due to its high prevalence, polymorphism, development of severe diseases and irreversibility of changes. Despite four options for algorithms and choice of insulin therapy, the difficult task of switching to the insulin resistance (IR) scheme due to the impossibility of using drugs from the biguanide and glitazone group, since their use in T1DM is not provided for by the instructions. The presented observation shows the clinical picture of IR against the background of metabolic syndrome and prolonged hyperglycemia in patients with T1DM and special attention is paid to the importance of prescribing adequate insulin therapy and an individual approach to patient management. The main strategy in this case is a gradual increase in the insulin dose until the target glycemic indicators are achieved. At the same time, after achieving adequate doses and the patient staying within the near-target indicators for a certain period of time, it is possible to use insulin restrictions against the background of neutralizing the effect of glucotoxicity on peripheral tissues.
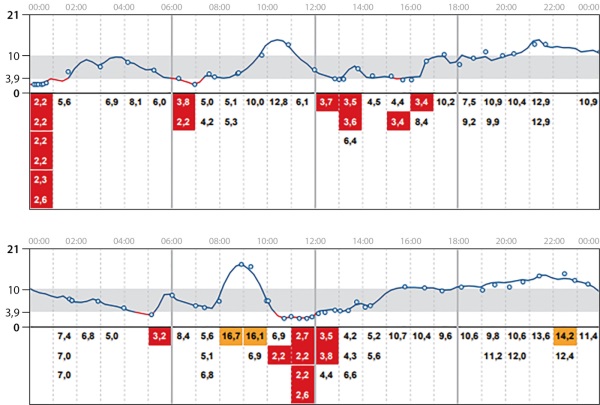
Artificial hypoglycemia (Munchausen syndrome) is a condition caused by low blood glucose due to the deliberate taking of insulin or oral hypoglycemic drugs. Artificial hypoglycemia remains one of the problems that endocrinologists face in their practice; a diagnostic search for its etiological factor can lead to expensive and unnecessary studies. Diagnosis of artificial hypoglycemia in patients with diabetes mellitus on insulin therapy seems to be a labor-intensive task, since unlike most factitious disorders, which may be indicated by atypical manifestations of the disease or conflicting medical information about the patient, in patients with diabetes mellitus hypoglycemic syndrome is an expected unwanted event due to insulin therapy. Therefore, deliberate insulin administration is often not diagnosed until self-induced hypoglycemia becomes recurrent and/or severe. If artificial hypoglycemia is suspected, a number of authors currently recommend testing С peptide and a combination of two methods for quantitative determination of insulin in the blood using different analyzer systems. Active collaboration between clinical and laboratory specialists is the key to successfully solving such a diagnostic problem.
This article presents a clinical case of Munchausen syndrome in a 28-year-old patient with type 1 diabetes mellitus with recurrent hypoglycemia during 21 years, repeated severe hypoglycemia, including loss of consciousness, and proven intentional administration of an insulin analog drug during hospital stay; the complex diagnostic path passed before making the correct diagnosis is described.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2072-0378 (Online)