Original Studies
BACKGROUND: In the treatment of diabetes mellitus (DM) for a persistent reduction in blood glucose levels it was widely used glibenclamide — a KATP channels blocker. However, its effects on cerebral circulation have been studied very little. A decrease in the functional activity of KATP channels due to their blocking by glibenclamide against the background of developed endothelial dysfunction may lead to impaired cerebral circulation (especially at the microcirculatory level) and promote remodeling of the vascular network.
AIM: To evaluate the effect of glibenclamide on the reactivity of cerebral arteries in rats with streptozotocin-induced diabetes mellitus (STZ-T2DM).
TASKS: 1. To study changes in the functional state of KATP channels of pial arteries in STZ-T2DM. 2. To evaluate the effect of glibenclamide on the participation of KATP channels in the formation of basal tone and endothelium-dependent dilatation of pial arteries.
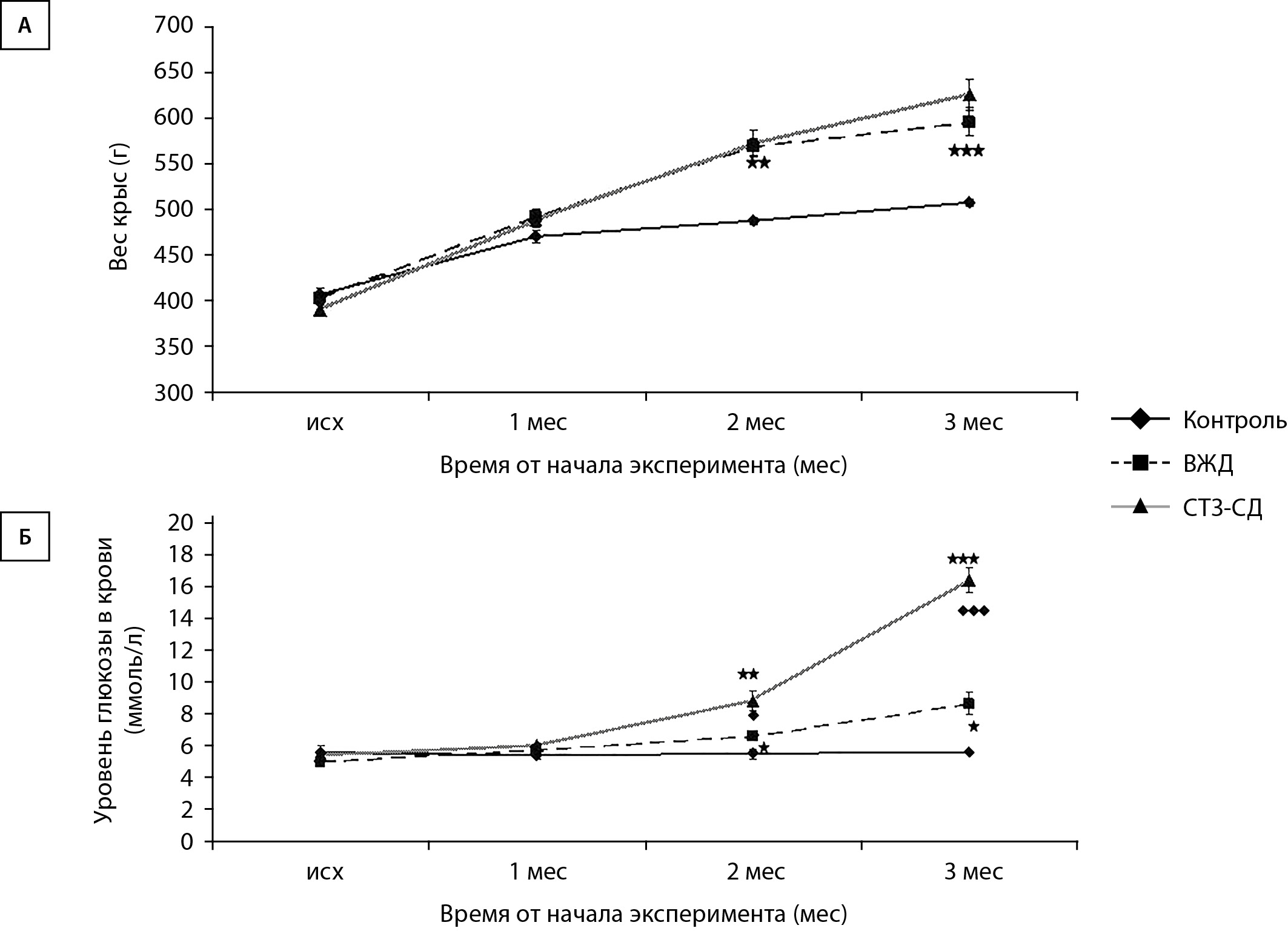
MATERIALS AND METHODS: The study was performed on 54 male Sprague Dawley rats. Streptozotocin-induced diabetes mellitus (STZ-T2DM) was modeled by keeping animals on a high-fat diet and administering streptozocin (35 mg/kg). Using an installation for intravital study of pial vessels reactivity, 3 months from the beginning of the experiment, the diameter of the arteries was measured when the brain surface was irrigated with Krebs-Henseleit solution, acetylcholine, glibenclamide, pinacidil and acetylcholine against the background of the action of glibenclamide or pinacidil.
RESULTS: With modeling STZ-T2DM, rats developed glucose tolerance and insulin resistance. Compared to control animals, body weight was 1,3 times higher, the percentage of visceral fat was 3 times higher, and the blood glucose level was 3,2 times higher. It was shown that in STZ-T2DM the number of pial artery constrictions under the action of glibenclamide decreased by 1,3 — 1,9 times compared to intact rats. Glibenclamide did not block endothelium-dependent dilation.
CONCLUSION: In rats with streptozotocin diabetes, KATP channels take part in the formation of the basal tone of the pial arteries, but the contribution of these channels is reduced on average by 1.5 times compared to healthy rats.
The use of glibenclamide in STZ-T2DM does not affect endothelium-dependent dilatation of cerebral arteries.
BACKGROUND: Type 1 diabetes mellitus (DM1) is a chronic autoimmune disease characterized by damage to insulin–producing cells of the pancreas, which eventually leads to the need for insulin replacement therapy. The clinical picture of DM1 is heterogeneous: the onset of the disease at an early age is characterized by a more acute manifestation and rapid depletion of residual insulin secretion. Variations of HLA genes can probably determine the clinical features of the course of DM1. To date, age-related features of HLA genes have been established in various populations, at the same time, such data are not available in the Russian population.
AIM: To study the effect of HLA genes on predisposition to DM1 in preschool age.
MATERIALS AND METHODS: A single-center, one-stage study, including data from 885 children (1 year — 18 years old) with previously diagnosed DM1 who are on intensified insulin therapy. The study participants’re divided into two groups: a group with a manifestation of DM1 <7 years and a group with a manifestation of DM1 ≥7 years. The age of diagnosis of DM1, SDS body mass index, glycated hemoglobin (HbA1c) and C-peptide levels, specific islet autoantibodies glutamate decarboxylase (GADA), tyrosine phosphase (IA-2A), zinc transporter (ZnT8A), HLA genes of classes I and II (NGS genotyping by high-performance sequencing) were analyzed.
RESULTS: In the group with manifestations of DM1 <7 years, lower levels of C-peptide’re detected (0 vs. 0.3 ng/ml, p<0.001), AT GAD was less often determined (48% vs. 67%, p=0.028), IA-2 (52% vs. 62%, p=0.014), ZnT8 (44% vs. 71%, p=0.002). There were no significant differences in the sex ratio, the level of HbA1c and SDS BMI. In the group with manifestations of DM1 <7 years, there was a high frequency of the most severe predisposing genotype DRB1*03-DQA1*05:01-DQB1*02:01 (DR3-DQ2)/DRB1*04-DQA1*03:01-DQB1*03:02 (DR4-DQ8) (27.5% vs 21.5%, p=0.039]) and a lower frequency of the protective haplotype DRB1*01-DQA1*01-DQB1*05:01 (19.1% vs. 24.9%, p=0.035). With respect to class I HLA genes, in the group with manifestation <7 years, there was a high frequency of predisposing haplotype A*24:02 (35.6% vs. 24.1%, p=0.002). Regardless of the age of onset and duration of the disease, the absence of residual C-peptide secretion (<0.1ng/ml) was associated with the presence of the predisposing haplotype DR4-DQ8 (65.7% vs. 60.8%, p=0.04) and B*18:01 (20.9% vs. 16.9%, p=0.026), and also with a lower frequency of tread haplotypes DRB1*15-DQA1*01:03-DQB1*06:03 or DRB1*15-DQA1*01:02-DQB1*06:02 (1.3% vs. 3.3%, p=0.047). The presence of IA-2A and ZnT8A was associated with the DR4-DQ8 haplotype (28.2% vs. 16.5%, p=0.037, and 33.3% vs. 15.4%, p=0.018, respectively). GADAs were associated with the predisposing haplotype DR3-DQ2 (55.0% vs. 34.5%, p=0.03).
CONCLUSION: Predisposing and protective HLA haplotypes of class I and II associated with the manifestation of DM1 in preschool age and the reserve function of beta cells have been established in the Russian population. The relationship of the presence of islet AT with predisposing DR3/DR4 haplotypes is shown, which can determine various mechanisms of formation and course of the autoimmune process.
BACKGROUND: Molecular genetic testing (MGT) is increasingly accessible, improving diagnosis of monogenic diabetes (DM), particularly maturity-onset diabetes of the young (MODY). While most MODY research focuses on pediatric populations, diagnosis is possible after age 18. The Federal Diabetes Registry (FDR) offers unique insights into real-world management of MODY patients.
AIM: To analyze the clinical features of DM onset, carbohydrate metabolism, complications, and hypoglycemic therapy (HT) in patients with the main types of MODY based on the FDR data.
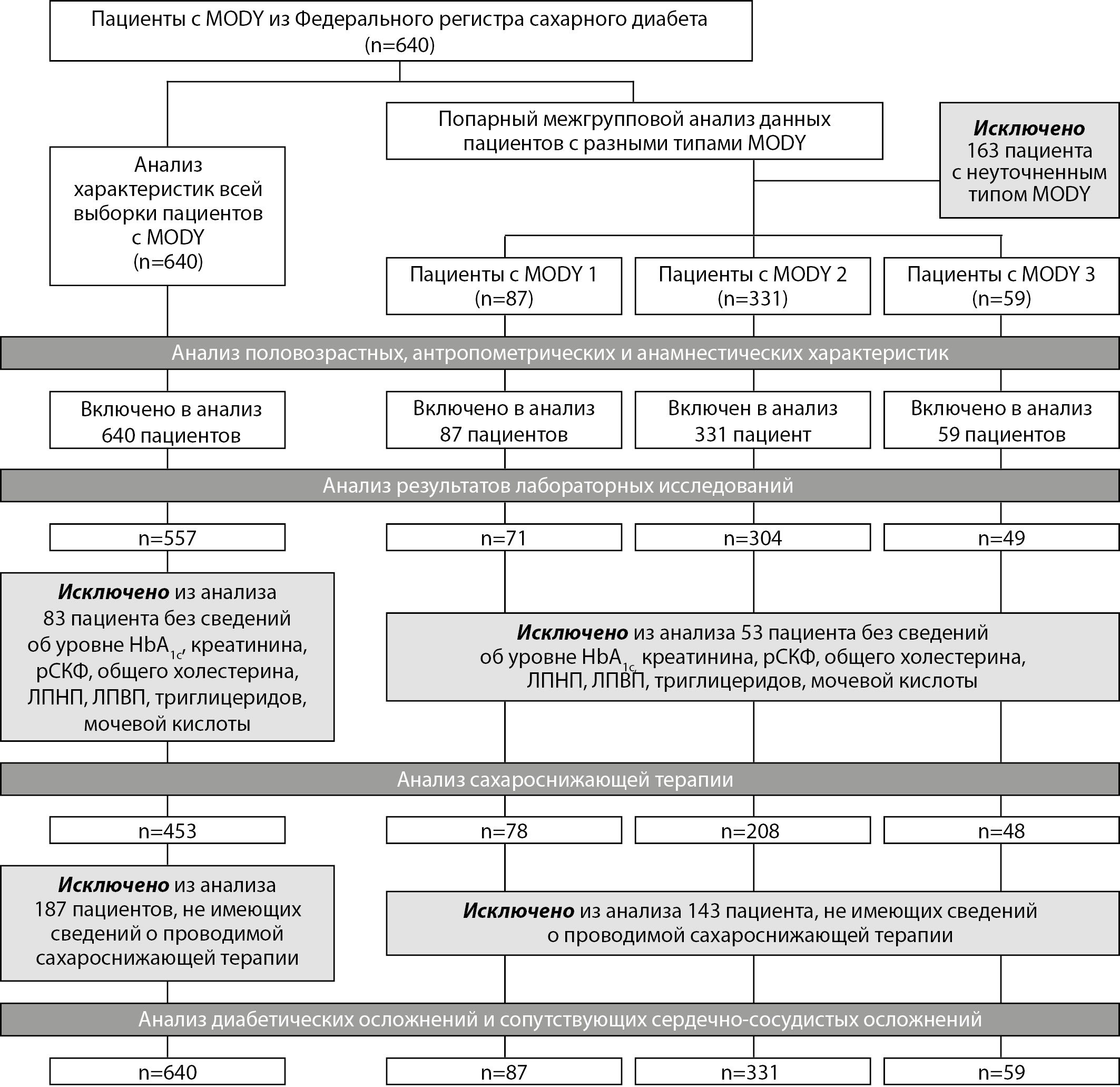
MATERIALS AND METHODS: A cross-sectional analysis of the FDR was conducted. All patients with registered MODY diagnoses (MODY-1, MODY-2, MODY-3, or other) as of June 1, 2023, were included. The specified MODY type was considered indicative of prior MGT. Direct MGT results are not recorded in the FDR.
RESULTS: The study included 640 patients. MODY2 was the most prevalent type (69.4%), followed by MODY1 (18.2%) and MODY3 (12.4%). The median age of DM diagnosis was 19 years for MODY1, 10 years for MODY2, and 14 years for MODY3. The majority of patients (71.4%) were diagnosed with MODY before the age of 18 years.
While 61% of MODY2 patients received monotherapy with diet, others received various ADT. Sulfonylureas were commonly prescribed for MODY3 patients (45.8%), and for a smaller portion of MODY1 patients (14.1%). Insulin therapy was more frequent in MODY1 and 3 (35.9% and 31.2%, respectively). The target glycated hemoglobin level was achieved in 82% of MODY2 patients and in 50.7% and 52.9% of MODY1 and 3 patients, respectively.
Diabetic complications were observed in 6.04% of MODY2 patients, 23.0% of MODY1 patients, and 22.0% of MODY3 patients. Specific complications included diabetic retinopathy (5.75%, 1.21%, and 3.39% in MODY1, MODY2, and MODY3, respectively), diabetic nephropathy (10.3%, 2.11%, and 11.9%), and diabetic polyneuropathy (14.9%, 4.53%, and 15.3%).
CONCLUSION: The FDR analysis revealed real-world practice patterns in MODY management, highlighting a lack of standardized treatment approaches and potentially unnecessary insulin use. These findings, coupled with an expected rise in MODY diagnoses, underscore the need for clinical guidelines for this population.
INTRODUCTION. Gestational diabetes mellitus (GDM) is one of the most common diseases during pregnancy. To date, there is evidence showing that not all pregnant women with GDM have the same risks of developing complications. Identification of patients at increased risk of complications may be necessary given the increasing prevalence of GDM. The need for a more detailed study of GDM subtypes to identify patients at high risk of complications formed the basis of the study.
PURPOSE. Determination of anamnestic, phenotypic, and biochemical characteristics of GDM subtypes for the further development of diagnostic and treatment methods.
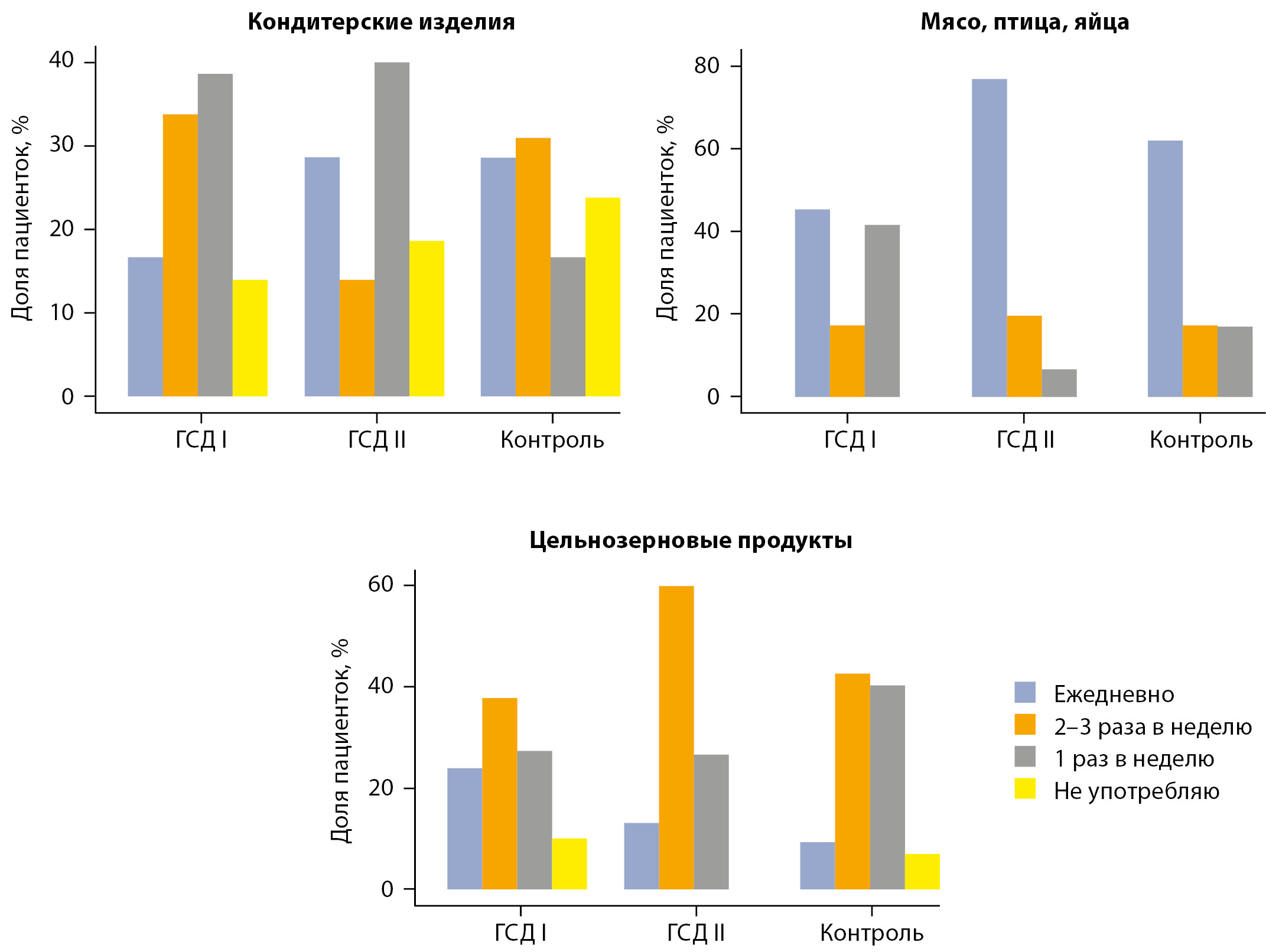
MATERIALS AND METHODS. A single-center observational prospective study was carried out at the Department of Internal Medicine No. 3 of the Rostov State Medical University of the Ministry of Health of the Russian Federation in the period from April 2021 to August 2022. The study included 130 pregnant women. Participants underwent an oral glucose tolerance test with 75 g of glucose assessing fasting, 60- and 120-minutes venous plasma glucose and insulin levels, and fasting blood was drawn to determine levels of main lipid metabolism indicators, apolipoprotein A, and apolipoprotein B, adiponectin, leptin and omentin, glycated hemoglobin, C-reactive protein. All study participants underwent anamnesis and physical examination with assessment of body mass index (BMI), blood pressure, signs of acanthosis nigricans, and a questionnaire. When GDM was detected, the Matsuda index was calculated: >50th percentile in comparison with the values of pregnant women without carbohydrate metabolism disorders, the patient belonged to the group of GDM with β-cell dysfunction; <50th percentile - to the GDM group with predominant insulin resistance.
RESULTS AND DISCUSSION. Women with GDM and insulin resistance were older, had a higher BMI before pregnancy, greater weight gain, and more often had signs of acanthosis nigricans compared to patients with GDM and β-cell dysfunction. Also, when comparing patients with different subtypes of GDM, numerous biochemical differences and lifestyle features were identified..
CONCLUSION. We demonstrated pronounced anamnestic, phenotypic, and biochemical heterogeneity in patients with different subtypes of GDM, which may become the basis for the further development of verification of GDM subtypes.
BACKGROUND: To date, the results of Metformin, Gosogliptin and combination thereof have not been studied on a large patient population with type 2 diabetes mellitus (DM2), including comorbid patients, in real clinical settings in the Russian Federation.
AIM: The aim is to evaluate the efficacy, safety, treatment adherence and satisfaction of patients with DM2 with the use of Metformin and Gosogliptin sugar-lowering drugs and combination thereof in routine clinical practice.
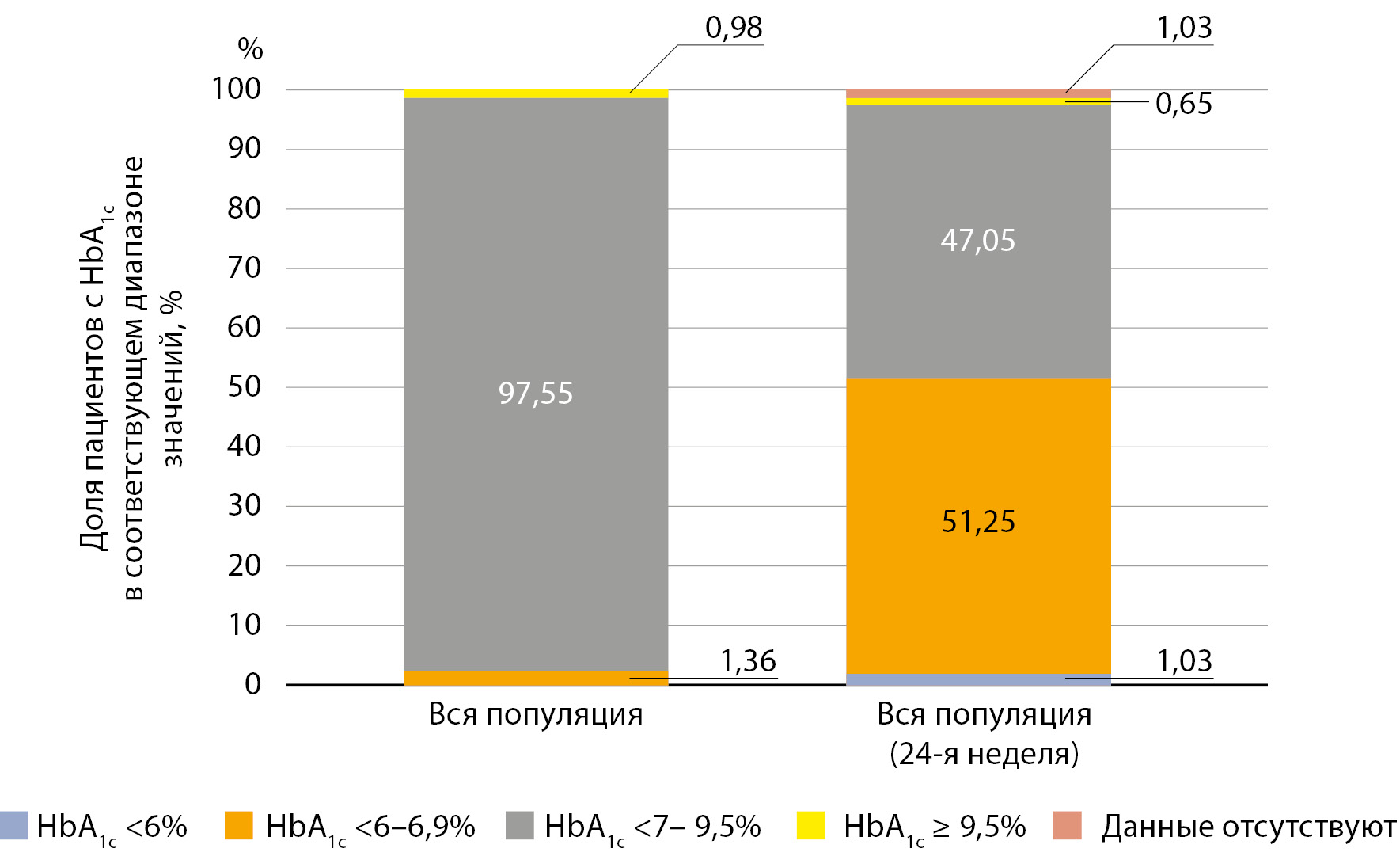
MATERIALS AND METHODS: The nationwide PALITRA multicenter observational study was conducted among patients with DM2 who were prescribed therapy with Metformin or Gosogliptin or combination thereof in everyday clinical practice. Groups were formed according to the sugar-lowering drug administered; a total of 5741 patients aged 18 to 65 years with DM2 and a wide comorbidity profile participated. The observation period was 6 months. Body weight, body mass index (BMI), blood pressure (BP), glycated hemoglobin (HbA1c) level, glycemic parameters, and biochemical parameters (ALT, AST and plasma creatinine) were recorded initially and 3 and 6 months after the initiation of therapy with the study drugs. Adherence to therapy and patient and physician satisfaction with the treatment were assessed using Likert scale.
RESULTS: HbA1c level decreased by 1.03% in the Metformin monotherapy group and by 0.95% in the Gosogliptin monotherapy and Metformin and Gosogliptin combination therapy groups by Week 24. By the end of the study, 49.6% of patients with DM2 reached the target HbA1c level (<7.0%). The proportion of patients with HbA1c level <7.0% was 61.0% in the Metformin group, 47.75% and 47.2% in the Gosogliptin and Metformin/Gosogliptin dual combination therapy groups, respectively. The incidence of hypoglycemic episodes was very low throughout the whole period of observation, during which body weight decreased slightly. High satisfaction of patients and physicians with DM2 treatment was shown. This was reflected by high Likert scale scores.
CONCLUSION: It has been proved that Metformin, Gosogliptin and the combination of Metformin and Gosogliptin were highly effective and safe (low incidence of hypoglycemia and no effect on body weight), and patients and physicians had been satisfied with the sugar-lowering therapy in a sufficient number of Russian patients with DM2 and a wide comorbidity profile.
BACKGROUND: Considering the role of visceral adipose tissue deposition in the pathogenesis of heart failure with preserved ejection fraction (HFpEF) and the positive effect of metformin on weight loss, the effect of this drug on adipose tissue compartments in patients with HFpEF is interest.
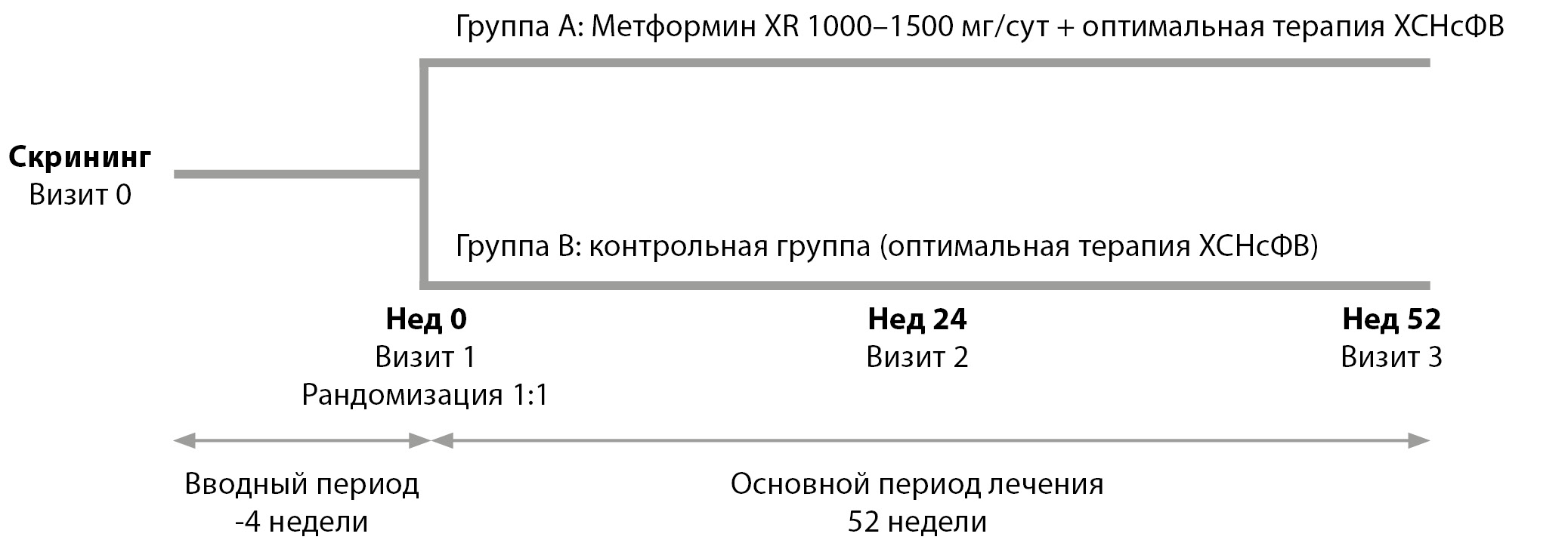
AIM: To study the effect of extended-release metformin (XR) on various fat depots and parameters of insulin-glucose homeostasis in patients with HFpEF, prediabetes and abdominal obesity (AO).
MATERIALS AND METHODS: Study design: single-center, open-ended, randomized, prospective, controlled. The registration numbers of the study in the NARNIS register RNI.25.004. The study included 64 people (50% men, median age 58 [55.25; 59.75] years) with HFpEF, prediabetes and AO. All patients (groups A and B) received optimal HFpEF therapy. In group A (n=32), metformin XR 1000–1500 mg/day was additionally prescribed. All patients underwent general clinical examination, calculation of insulin resistance indices, ultrasound lipometry to determine the thickness of epicardial, preperitoneal and subcutaneous fat initially and after 6 months.
RESULTS: In group A patients, there was a decrease in waist circumference by 0.9% (p=0.002), hip circumference by 1.25% (p=0.001), body weight by 4.7% (p<0.0001), body mass index by 1.8% (p=0.001) compared with baseline. In the control group, the anthropometric parameters of the dynamics did not change. Also, in the metformin XR group, glucose levels decreased by 4.6% (p=0.009), glycated hemoglobin by 3.3% (p=0.047), insulin by 12.5% (p=0.024) and insulin resistance indices: HOMA-IR by 19.8% (p=0.009), FIRI by 19.8% (p=0.009). In contrast, patients from group B had an increase in fasting plasma insulin levels by 33.6% (p=0.035), with an increase in HOMA-IR indices by 27.4% (p=0.026) and FIRI by 26.9% (p=0.025). The dynamics of ultrasound lipometry parameters was observed only in group A: the thickness of the preperitoneal fat decreased by 14.5% (p<0.0001), the thickness of the subcutaneous fat decreased by 12.3% (p<0.0001).
CONCLUSION: In patients with prediabetes, HFpEF and AO, taking metformin XR 1000-1500 mg/day for 6 months against the background of optimal basic HFpEF therapy was associated with a decrease in subcutaneous and preperitoneal fat, also had a beneficial effect on glucose metabolism parameters compared with the control group.
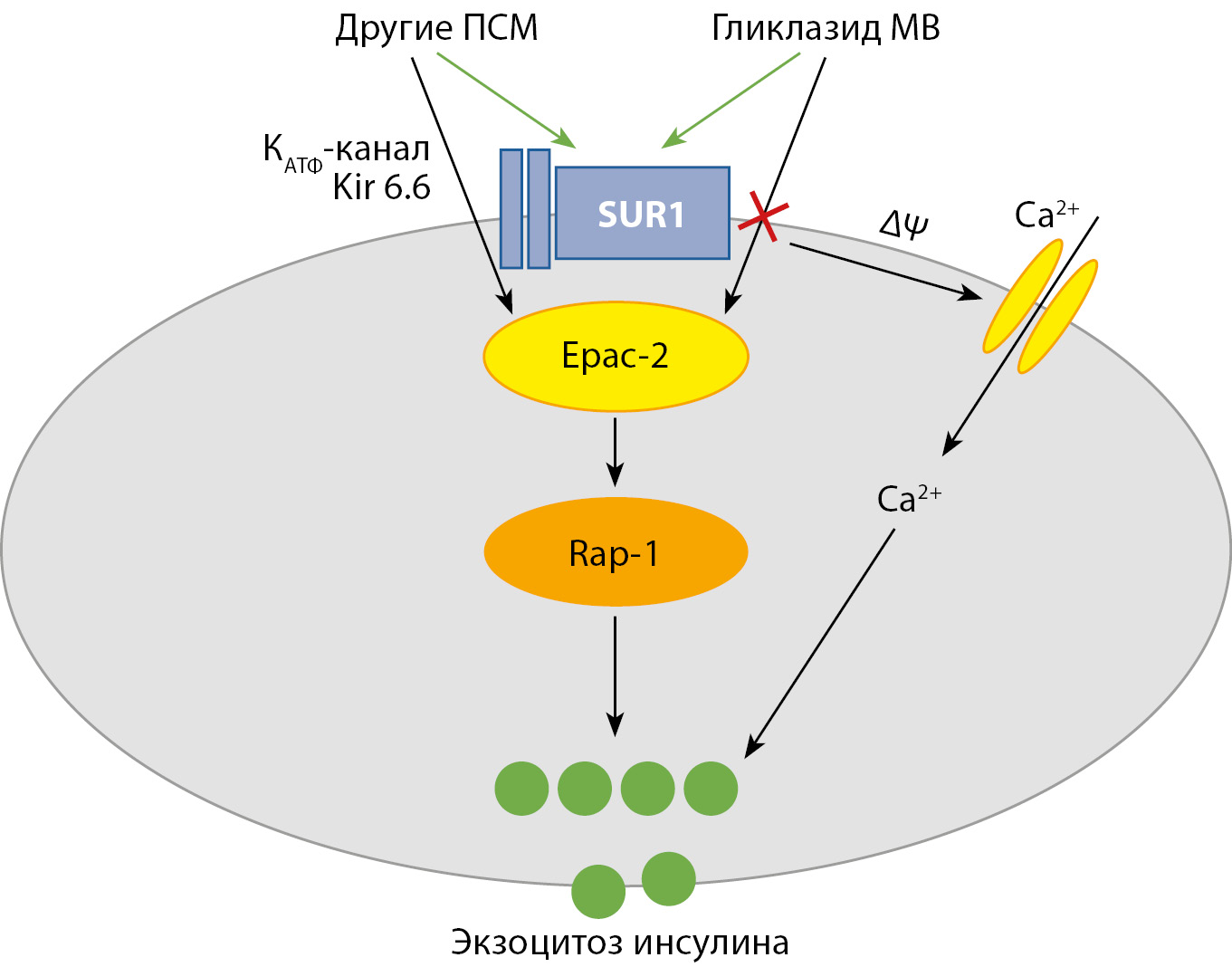
Sulfonylurea (SU) are an effective class of oral hypoglycemic drugs that have been used in clinical practice for more than 70 years. Despite the common mechanism of action, members of the class have significant intraclass differences in hypoglycemic activity, safety, and the presence of extrapancreatic effects. This review examines the features of gliclazide modified release (MR), its differences from other representatives of the SU and its place in modern recommendations for the treatment of type 2 diabetes mellitus. Gliclazide MR belongs to the modern 2nd generation SU with high hypoglycemic activity, low risk of hypoglycemia due to reversible binding to the SUR1 receptor and no effect on the Epac2 pathway, generally neutral effect on weight, proven nephroprotective properties and cardiovascular safety, which makes it possible to highlight it among representatives of the SU class. International and national clinical guidelines indicate the place of SU when it is necessary to intensify glucose-lowering therapy and glycemic control in patients with type 2 diabetes mellitus.
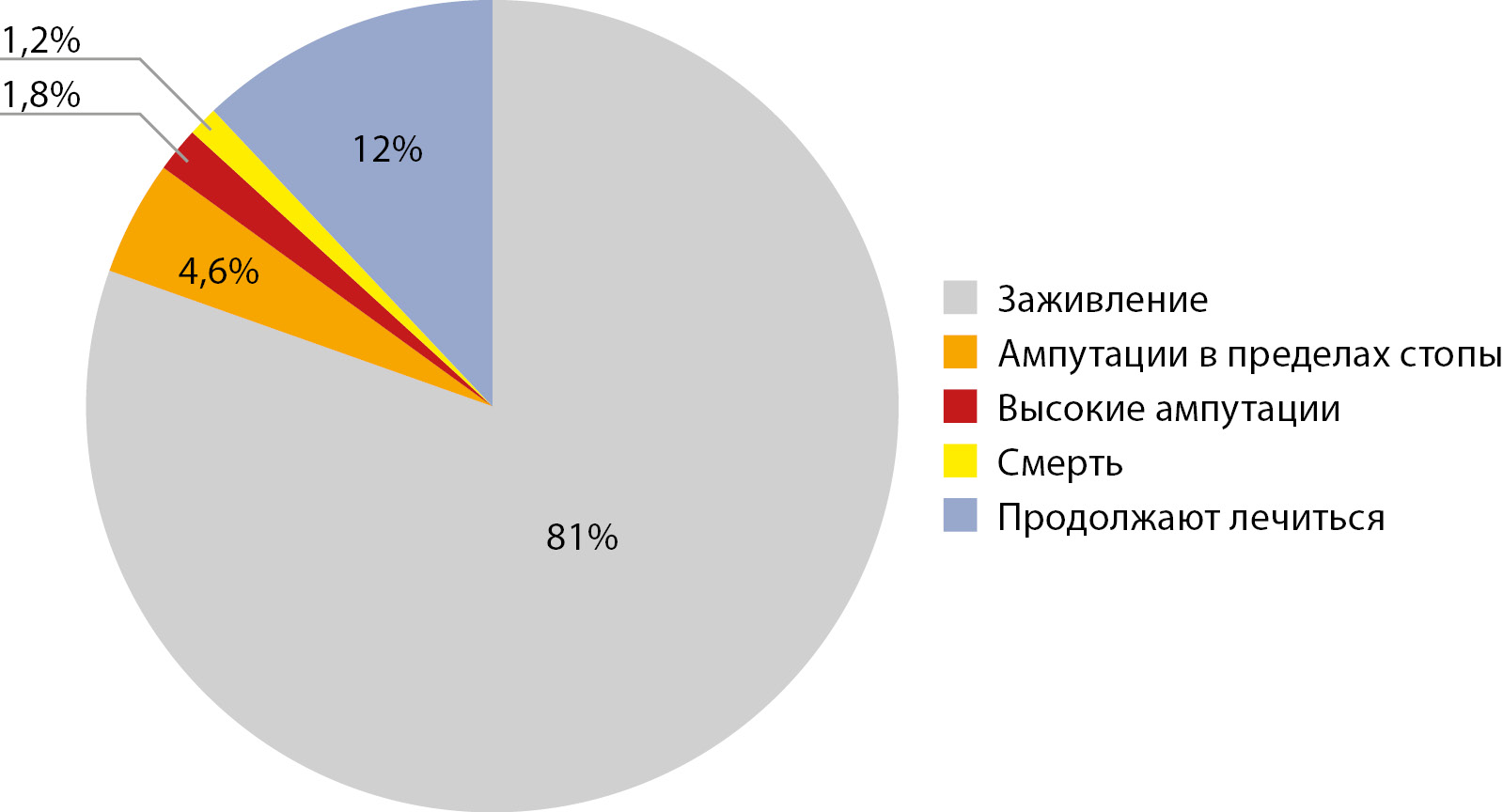
BACKGROUND: Diabetic foot syndrome is a late complication of diabetes mellitus and the main reason for non-traumatic amputations of the lower extremities in diabetic patients. Currently, standards of medical care have been developed and implemented for the treatment and prevention of this complication. At the same time, there is a lack of publications on the effectiveness of specialized care, especially at the pre-hospital stage.
AIM: To analyze the results of treatment of patients with diabetic foot on an outpatient basis in a specialized department and identify the factors affecting them.
MATERIALS AND METHODS: Medical records of patients with diabetic foot ulcers receiving specialized outpatient treatment in the diabetic foot department were analyzed. All patients underwent an assessment of the peripheral sensitivity and blood flow of low extremities during the initial examination. Treatment was prescribed in accordance with the presence and severity of infection and ischemia of the affected limb. The number of amputations at different levels, the percentage of healed and unhealed wounds during the year were analyzed. Predictors of high amputations and non healing during the year were identified.
RESULTS: Out of 503 patients with diabetic foot, neuropathic diabetic foot was diagnosed in 336 (67%) patients, neuro-ischemic in 167 (33%). Healing without amputations in the general cohort of patients was noted in 407 cases (81%). In 32 (7%) cases, amputations were required, of which: 23 (5%) within the foot, 3 above ankle (0.6%), 6 above knee (1.2%). Death occurred in 6 patients (1.2%), 2 of them after hip amputation. 61 patients (12%) continued to be treated at the end of the study. The predictors of high amputations in the general cohort of patients were age, impaired arterial blood flow in the arteries of the lower extremities, the depth of the Wagner ulcer and the level of glycated hemoglobin. Predictors of the non healing during the year were: the presence of impaired arterial blood flow and untimely treatment for specialized medical care.
CONCLUSION: The data obtained demonstrated the high effectiveness of specialized care for patients with diabetic foot ulcers at the prehospital stage
Review
Diabetic Charcot neuroosteoarthropathy is a manifestation of diabetic foot syndrome, accompanied by a high risk of foot ulcers and amputation. Many aspects of this pathology due to its features remain poorly understood, which leads to difficulties in determining the tactics of treatment of these patients. This review analyzes of anatomical and functional classifications of Charcot foot. The review focuses on the midfoot pathology as the most severe in their consequences. The advantages and disadvantages of different approaches to the description of the X-ray picture of the disease at its various stages are analyzed. The systematization of the literature allows us to conclude that the existing approaches to classification are relatively acceptable mainly when planning conservative treatment. At the same time, detailed anatomical and radiological classifications do not help in choosing the tactics of reconstructive surgical treatment. With the increasing availability of reconstructive surgery for severe deformities due to Charcot’s arthropathy, it seems appropriate to develop classification systems that could become a practical tool for determining surgical tactics in this pathology.
Case report
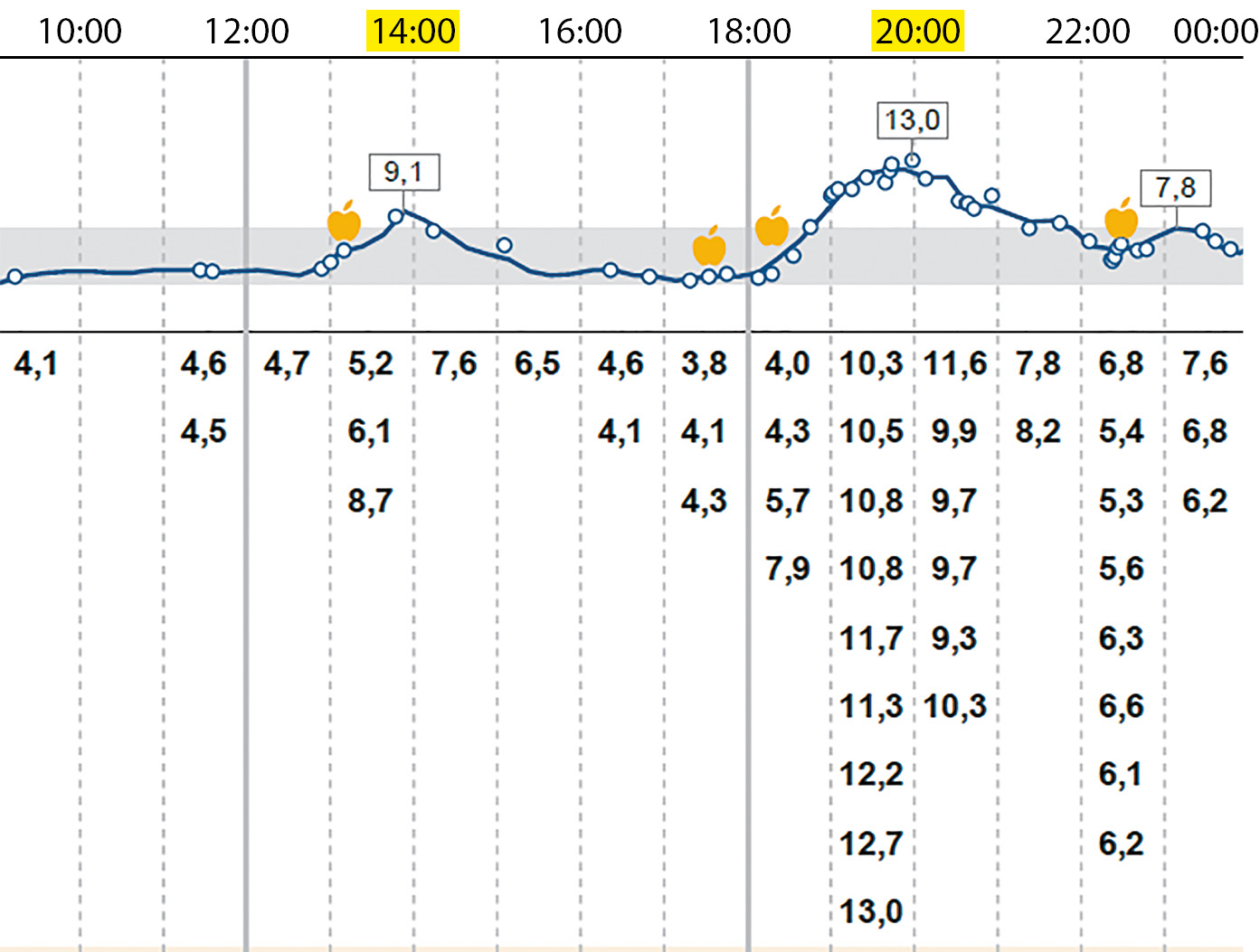
Women of reproductive age with type 1 diabetes mellitus (DM) and chronic kidney disease stage 5 after successful combined pancreas-kidney transplantation (CPKT) can experience spontaneous pregnancies with a favorable outcome. However, those pregnancies are associated with a high risk of complications: arterial hypertension, preeclampsia, premature birth, progression of diabetic retinopathy. During pregnancy, both gestational diabetes and spontaneous hypoglycemia can develop. This article presents a description of the clinical case of a 42-year-old patient with DM type 1, in whom pregnancy occurred 2 years after successful CPKT. Blood pressure was normal, the fundus condition was stable after previous treatment. The patient received tacrolimus and minimal dose of corticosteroids, at 13 weeks acetylsalicylic acid was prescribed to prevent preeclampsia. At 30 weeks nocturnal episodes of hypoglycemia appeared that were treated by additional intake of carbohydrates with an average glycemic index in combination with animal fats and proteins. At 36 gestational weeks caesarean section was performed due to premature rupture of membranes. A healthy girl was born with weight of 2140 g, height of 48 cm, Apgar score 7/8 points. The mother’s function of the kidney and pancreas grafts remained normal. Preconceptional counseling and multidisciplinary pregnancy management are important for patients after CPKT.
Erratum
An erratum on « Insufficiency/deficiency of vitamin B12 in patients in the endocrinological practice» by Natalya G. Mokrysheva, Marina V. Shestakova, Alexander S. Ametov, Mikhail B. Antsiferov, Igor G. Bakulin, Tatiana V. Vavilova, Gagik R. Galstyan, Tatiana Y. Demidova, Fatima K. Dzgoeva, Tatiana L. Karonova, Elena A. Lukina, Ashot M. Mkrtumyan, Rodion V. Ponomaryov, Natalia A. Suponeva, Olga Y. Sukhareva, Minara S. Shamkhalova (2024). Diabetes mellitus. 27(3). doi: 10.14341/DM13181
An error was made in the list of authors: Nina A. Petunina was not indicated as author of this article. The correct list of authors: Natalya G. Mokrysheva, Marina V. Shestakova, Alexander S. Ametov, Mikhail B. Antsiferov, Igor G. Bakulin, Tatiana V. Vavilova, Gagik R. Galstyan, Tatiana Y. Demidova, Fatima K. Dzgoeva, Tatiana L. Karonova, Elena A. Lukina, Ashot M. Mkrtumyan, Nina A. Petunina, Rodion V. Ponomaryov, Natalia A. Suponeva, Olga Y. Sukhareva, Minara S. Shamkhalova.
The identifier in the ORCID system for F.K. Dzgoeva was also indicated incorrectly. The correct link is: https://orcid.org/0000-0002-0533-7652.
The editorial board apologize for this error and state that this does not change the scientific conclusions of the article in any way.
The original article has been updated.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2072-0378 (Online)