Original Studies
BACKGROUND: Bariatric surgery (BS) is one of the most effective treatment strategies for patients with morbid obesity and type 2 diabetes (T2DM). More than 80% of patients not only lose weight after BS, but also achieve T2DM remission. However, weight regain and T2DM relapse can occur in the long-term (>5–10 yrs).
AIM: The purpose of the study was to assess the risk factors for T2DM relapse and weight regain ≥5 yrs. after BS.
MATERIALS AND METHODS: The study included 111 patients with obesity and T2DM who underwent BS: sleeve gas trectomy/gastric bypass/SADI/ BPD/DS ≥5 yrs. after BS. All the patients were analyzed according to the two main criteria: weight maintenance and stability of diabetes remission. The T2DM remission criteria were HbA1c≤6.5% and FPG<7.0 mmol/l for at least 3 months after antidiabetic therapy withdrawal. The weight maintenance criterion was an increase of <10 kg from nadir.
RESULTS: The patients were divided twice into groups with stable weight loss and its maintenance (group 1) vs. weight regain (group 2) and stable T2DM remission (group 3) vs. T2DM relapse (group 4). There were no significant differences be tween Gr.1 and Gr.2 in preoperative characteristics. In Gr. 4 compared to Gr.3 there were statistically significant differences in preoperative HbA1c (8.70% vs. 7.45%, p<0.001), basal insulin levels (12.70 vs. 28.1 μIU/ml, p<0.001), preoperative C-peptide (3.01 vs. 4.72 ng/ml, p<0.001), T2DM duration (9 vs. 4 yrs., p<0.001), frequency of insulin therapy and multiple hypoglycemic therapy.
CONCLUSION: Risk factors for T2DM relapse included: longer duration of T2DM, higher preoperative HbA1c levels, lower baseline insulin and C-peptide levels, insulin therapy and multiple hypoglycemic therapy. Statistically significant relationship between T2DM relapse and weight regain after BS, as well as their connection with BS type were not found in our study and require further investigation.
BACKGROUND: Type 1 diabetes mellitus (DM1) is a chronic disease, the main causes of disability, mortality and decreased quality of life in which are acute and chronic complications. The onset of T1DM in childhood is associated with a significant reduction in life expectancy and a higher risk of cardiovascular complications. In addition, the chronic course of T1DM is often accompanied by other autoimmune diseases (autoimmune thyroiditis (AIT), celiac disease), as well as concomitant conditions (growth retardation, dyslipidemia, etc.), which have independent significance.
AIM: To assess the frequency and provide clinical characteristics of complications, concomitant diseases and conditions in children with T1DM who fell ill during preschool age.
MATERIALS AND METHODS: A single-center, cross-sectional study including data from 396 children aged 4 to 18 years with previously diagnosed T1DM, according to generally accepted criteria, for a duration of at least 3 and no more than 10 years on intensified insulintherapy. Depending on the age of diagnosis of T1DM, study participants were divided into two groups: group with manifestation of T1DM <7 years and group with manifestation of T1DM ≥7 years.
RESULTS: Median age was 11.9 [9.3; 14.9] years, disease duration 5.2 [3.9; 6.9] years, glycated hemoglobin level 7.9 [7.2; 9.2] %. Study groups did not differ in gender, disease duration or SDS BMI. The level of glycated hemoglobin (p=0.011) and height SDS (p=0.041) were higher in children with onset of T1DM over 7 years of age. According to the results of regression analysis, taking into account the correction for the age of children at the time of examination, a direct relationship was established between the manifestation of T1DM in preschool age and retinopathy (β=4.95), MAU (β=2.64) and growth retardation (height SDS less than 2 ) (β=1.22). In contrast, a decrease in GFR was associated with an older age at onset of T1DM (p=0.012). After adjustment for age, the incidence of AIT, celiac disease and dyslipidemia did not differ significantly depending on the age of diagnosis of T1DM.
CONCLUSION: The data obtained indicate the importance of the manifestation of T1DM in preschool age as an independent risk factor for vascular complications in children and slower linear growth. Although the exact causes are not fully understood today, these data indicatethe need for more careful and strict monitoring of T1DM in young children, starting from the very onset of the disease.
BACKGROUND: Deintensification of basal-bolus insulin therapy (BBIT) with simplification of the treatment regimen is a possible and necessary therapeutic strategy for some patients with type 2 diabetes (T2D). One of the options for deintensification is the transition to fixed combination of insulin glargine/lixisenatide (iGlarLixi).
AIM: To determine the efficacy and safety of deintensification of BBIT in hospitalized patients with T2D by switching to iGlarLixi under continuous glucose monitoring (CGM).
MATERIALS AND METHODS: Design: single-center, comparative, observational study in real-world settings. A total of 283 T2D patients on BBIT were included, 118 subjects underwent BBIT deintensification under CGM control according to clinical indications, 165 patients continued BBIT. Thirty patients were re-examined one year after deintensification. Time In target Range (TIR), Time Above Range (TAR), Time Below Range (TBR), as well as Coefficient of Variation (CV), Mean Amplitude of Glycemic Excursions (MAGE), Lability Index (LI), and Mean Absolute Glucose rate of change (MAG) were estimated. Endogenous insulin secretion was assessed by fasting and 2-hour postprandial C-peptide levels. The estimated glucose disposal rate (eGDR) was used as a measure of insulin sensitivity.
RESULTS: The groups were similar in age, diabetes duration, glycated hemoglobin (HbA1c) and eGDR. Body mass index (BMI) and C-peptide levels were higher, while the duration of insulin therapy and initial daily insulin dose (DID) were lower in patients of the deintensification group (all p<0.0004). During deintensification, DID was reduced (from 64 to 30 U/day, p<0.001). The achieved TIR and TBR values did not differ in two groups. In patients on iGlarLixi, TAR L2 (>13.9 mmol/L), CV, MAGE and MAG were lower (all p<0.05). In multivariate regression analysis, BMI, DID and fasting C-peptide were associated with successful deintensification. In ROC analysis, fasting C-peptide was the best predictor with a cut-off point of 0.92 ng/mL. One year after the treatment deintensification, there was a decrease in HbA1c (-0.5%, p=0.001) and body weight (-0.8 kg, p=0.003) and an increase in postprandial C-peptide levels (p=0.029) without changes in eGDR.
CONCLUSION: Switching to iGlarLixie is an effective therapeutic option for patients with T2D with normal C-peptide levels who require deintensification of BBIT.
BACKGROUND. Type 2 diabetes mellitus (T2DM) and diseases of the circulatory system continue to be one of the important health problems, given their high prevalence and comorbidity. Acute ST-segment elevation myocardial infarction (STEMI) in type 2 patients (T2DM) is characterized by a severe course with adverse clinical outcomes. Currently, the features of STEMI in patients with T2DM in different ethnic groups remain insufficiently studied.
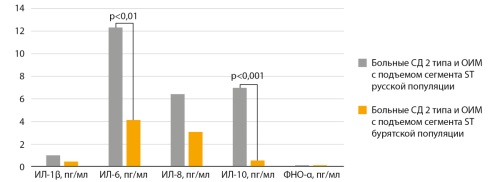
AIM. To determine the patterns of inflammatory response in patients with type 2 diabetes mellitus and acute ST-segment elevation myocardial infarction in the Buryat population.
MATERIALS AND METHODS. An observational single-center simultaneous comparative study was conducted on the basis of the Department of Endocrinology of IGMAPO, a branch of the Federal State Budgetary Educational Institution of the Russian Ministry of Health, and the N.A. Semashko Republican Clinical Hospital in Ulan-Ude of the Ministry of Health of the Republic of Buryatia. The study included patients with T2DM and STEMI with the participation of a control group. Anamnesis was collected from all participants of the study, and a clinical and functional examination was performed. In all subjects, serum levels of interleukin-1β (IL-1β), interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-10 (IL-10), tumor necrosis factor-α (TNF-α) were detected by the method of solid-phase enzyme immunoassay, while the immunoturbidimetric method was used to detect the level of high-sensitivity C-reactive protein (hs-CRP). In patients with T2DM and STEMI, venous blood sampling was performed on an empty stomach in the first 24 hours after the development of an angina attack.
RESULTS. The study included 77 people who were divided into patients of the Russian and Buryat populations, depending on their ethnic status. The group of the Russian population consisted of 21 patients with T2DM and STEMI and 22 people in the control group. The Buryat population group included 14 patients with T2DM and STEMI and 20 people in the control group. Russian population showed an increase in inflammatory response parameters (IL-1β, IL-6, IL-10, TNF-α, hs-CRP) in patients with T2DM and STEMI relative to the control group of the Russian population (p<0.01). There was registered a significant increase in the levels of IL-1β, IL-6 and hs-CRP in patients with T2DM and STEMI in the Buryat population compared with the indicators of the control group of Buryats (p<0.05). Comparative analysis showed that patients with T2DM and STEMI in the Buryat population are characterized by a decrease in the inflammatory response with cytokine decrease, both pro-inflammatory (IL-6) and anti-inflammatory (IL-10) against the background of a decrease in hs-CRP, relative to patients with T2DM and STEMI in the Russian population (p<0.05).
CONCLUSION. The results obtained indicate an imbalance of the cytokine system on the first day of the acute period in patients of the Buryat population with T2DM and STEMI against the background of a decrease in the anti-inflammatory link relative to patients with T2DM and STEMI in the Russian population.
BACKGROUND: Smoking disrupts the endocrine system, altering levels of key hormones such as estrogen (E2) and prolactin (PRL). This makes the relationship between smoking and sex hormones an important research topic. IL-12 is a crucial cytokine that enhances immune responses, particularly in promoting T-cell differentiation. AIM: This study aims to assess the impact of smoking on immune function by analyzing the reduction of pro-inflammatory cytokines (e.g., IL-12) and determining whether hormonal differences exacerbate this effect in females.
MATERIALS AND METHODS: Ninety serum samples were collected from healthy single females, age range (20–29) years old. The samples were divided into three groups: smokers (n=30), secondhand smokers (individuals exposed to tobacco smoke in their environment) (n=30), and non-smokers (control group, n=30). The female smokers were subdivided into 2 sub-groups: the first is based on the rate of smoking per day into heavy and light smokers, and the second group is the duration of smoking years (<4 years) and (≥4 years).
RESULTS: The findings revealed notable variations in the levels of IL-12, PRL, and HbA1c across all the studied groups (p-value <0.05). While, for E2, the (Median=92.68) in the smokers is lower than the control and secondhand smokers groups, the difference is non-significant.
CONCLUSION: Our findings suggest that heavy smoking adversely affects both metabolic health (increases HbA1c level) and hormonal balance in women. Also, smoking does decrease IL-12 levels, which can impair immune responses and affect overall health. While the durations of smoking (short-term vs. long-term) did not lead to notable changes in the outcomes being measured.
Review
To mark the 20th anniversary of clinical use of dipeptidase-4 inhibitors (DPP-4i), the understanding of the spectrum of effects (metabolic, clinical, biological) beyond the initially defined glycemic control is expanded, and the possibilities and directions of their safe use are considered, taking into account new biological effects. The cardiovascular and nephrological safety of DPP-4i is clarified in the context of combination therapy with metformin and insulin. The underestimated relationship between type 2 diabetes mellitus and bone fragility and the choice of antihyperglycemic drugs is analyzed. New biological effects of DPP-4 inhibitors with potential clinical significance are considered. Alogliptin is presented as an antidiabetic incretin agent with its capabilities and surprises in metabolic control.
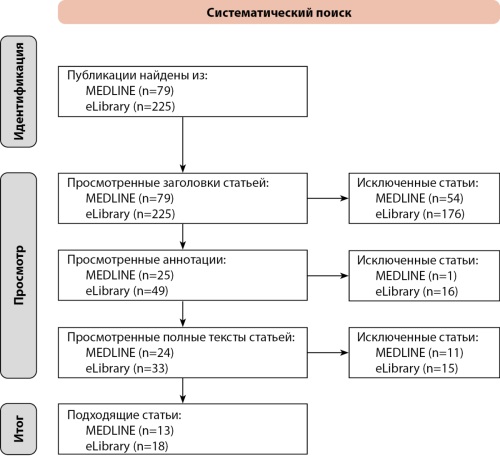
Diabetic retinopathy (DR) is one of the most common and severe complications of diabetes mellitus, often leading to blindness. Given the high prevalence of the disease and the limited capacity of ophthalmology services, the implementation of automated systems for early detection and monitoring of DR is becoming increasingly important. This review focuses on current advances in the application of computer vision and artificial intelligence (AI) techniques for DR diagnosis. A systematic search was conducted, followed by an analysis of 31 studies describing various approaches, including convolutional neural networks, pathology segmentation methods for fundus images, hybrid algorithms, and mobile applications for screening. Key features, model architectures, sensitivity and specificity metrics, as well as datasets used, are discussed. Special attention is given to AI systems already integrated into clinical practice, such as IDx-DR and EyeArt, which have received regulatory approval. The review highlights the importance of model interpretability, training data diversity, and image standardization as critical factors for improving the generalizability and trustworthiness of AI systems in ophthalmology. A distinctive aspect of this work is its comprehensive coverage of both international and Russian developments, including an assessment of their integration potential within the Russian healthcare system. The review concludes that several technologies have reached a level of maturity suitable for clinical use, while emphasizing the need for further research to enhance the accuracy, robustness, and transparency of diagnostic algorithms.
Brain natriuretic peptide (BNP) and N-terminal pro-brain natriuretic peptide (NT-proBNP) are polypeptide hormones released by cardiomyocytes in response to cardiac volume or pressure overload. The results of numerous studies have demonstrated the importance of these biomarkers for the diagnosis of chronic heart failure (CHF), including studies in patients with type 2 diabetes mellitus (T2DM). It has also been shown that the elevated BNP/NT-proBNP levels are associated with an unfavorable prognosis, and a decrease in the level of biomarkers over time can lead to a reduced incidence of fatal and non-fatal cardiovascular outcomes, as well as death from any cause. To date, the threshold values of BNP/NT-proBNP for the diagnosis of CHF, especially the phenotype of CHF with preserved left ventricular ejection fraction (CHFpEF), remain a subject of discussion, since the level of these biomarkers can be influenced by age, body mass index (BMI), kidney function, insulin resistance, acute and chronic inflammation. The aim of this review is to summarize the existing data on the clinical significance of BNP/ NT-proBNP monitoring with a focus on patients with T2DM and on factors that may influence the concentration of these biomarkers in the blood. The use of individual BNP/NT-proBNP cut-off values to improve the diagnostic accuracy of both asymptomatic cardiac dysfunction and overt CHF represents a promising area for further research.
Case report
Cadaveric kidney allotransplantation remains the most effective and safest therapeutic option for end-stage renal disease in patients with diabetes mellitus. Successful graft survival requires consideration of multiple factors that may contribute to transplant injury. Particular emphasis should be placed on minimizing the risk of transplant-associated infectious complications arising in the context of immunosuppressive therapy. We report a clinical case of kidney graft rejection in a female patient, occurring shortly after an episode of acute pyelonephritis and subsequent repeat cadaveric kidney allotransplantation.
Erratum
An error was identified in the article “A clinical case of pregnancy of a patient with a combination of two orphan diseases: familial partial lipodystrophy type 4 and HNF1A-MODY on the background of therapy with recombinant human methionyl leptin” by Frolkova N.V., Radkevich E.R., Koksharova E.O., Burumkulova F.F., Vasiliev P.A., Minniakhmetov I.R., Eremina I.A., Shestakova M.V., published in Diabetes mellitus. 2025;28(3):305-315. doi: https://doi.org/10.14341/DM13333. An error was made in the article: the source of funding was incorrectly indicated in the final text. The correct funding source is: This work was carried out within the framework of the state assignment «Model for personalized risk prediction of diabetes mellitus in children based on molecular genetic markers in ethnic groups of the Russian Federation and in familial cases of the disease,» state registration number 123021000040-9.
Jubilee Greetings

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2072-0378 (Online)