Scroll to:
Ethnopharmacological Insights into Diabetes Management: Exploring Medicinal Flora of Shivalik range of Himalaya in Uttarakhand
https://doi.org/10.14341/DM13080
Abstract
Diabetes mellitus is a chronic metabolic disorder which is commonly found life-threatening disease and it continuously reducing the life expectancy. It is characterized by hyperglycaemia (raised blood sugar level) resulting from defects in insulin secretion, action, or both. Since thousands of years, medicinal plants are being used by our ancestors for the prevention, treatment or even cure the diabetes mellitus. Utilization of these herbal plants is increasing rapidly last two to three decades due to their lesser toxicity and cost effectiveness property as compared to synthetic drugs. In this review, approximately 30 medicinal plants were described which are native to India and traditionally used by the people living in shivalik range of Himalaya in Uttarakhand (specially Dehradun & Haridwar) for the treatment of diabetes mellitus. The data about these plants was collected from science direct, PubMed, web of science, scopus, mdpi, google scholar and different other search engines and websites. This review was conferred in a systematic way as it includes botanical name, family, vernacular name, parts used and pharmacological uses of plants in a tabulated form. There are various scientific evidences behind the uses of some medicinal plants which have been mentioned along with the summary of individual medicinal plant. In this review, all the plants and herbs are easily available in these regions of Uttarakhand and local people traditionally uses these plants as vegetable, seasoning, flavouring and usually consume as a part of their diet. There are some limitations of phytotherapy which limit it to completely replace the allopathic therapy as less bioavailability, less rate of absorption and slow rate of dissolution. But by using various advanced dosage forms (phytosomes, neosomes, liposomes, nanoparticles, nanobubbles, nano diamonds, nanosphere etc.) and method of delivery (various invasive and non-invasive methods) which can bypass these all problems associated with the potency and efficacy of phytochemicals.
Keywords
For citations:
Kumar S., Kumar A., Tantray J., Shukla A. Ethnopharmacological Insights into Diabetes Management: Exploring Medicinal Flora of Shivalik range of Himalaya in Uttarakhand. Diabetes mellitus. 2024;27(5):498-509. https://doi.org/10.14341/DM13080
INTRODUCTION
In India, the WHO estimates that there are 77 million adults (those over the age of 18) who have type II diabetes and another 25 million prediabetics who are at risk of developing this condition in near future [1]. And according to a report by Sanyukta Kanwal that was published in Statista, more than 74 million Indians had been diagnosed with diabetes as of 2021, and that number is projected to increase to more than 124 million by 2045 [2]. Whereas as per 10th IDF Diabetes Atlas, there are 536.6 million peoples suffering with diabetes in the world till 2021 and this data will increase up to 783.2 million in 2045 [3]. Data may vary study to study but all the study concluded it surely that diabetes is a big matter of concern. For a number of reasons, we have decided to review the native Indian flora as a potential source of glucose-lowering compounds. First of all, native populations in focused area have a long history of using herbal medicine, and they frequently have extensive knowledge of therapeutic herbs and their uses. Second, investigating the local flora is consistent with the ideas of ethnopharmacology, which stresses the study of traditional medical practices in search of possible therapeutic advantages. For systematic literature review, we employed a systematic approach to search, evaluate, and select references for this review. Firstly, we have conducted comprehensive literature searches using electronic databases such as Web of Science, Scopus, Science direct, PubMed, PubMed central, mdpi, Google Scholar, and relevant botanical databases. Keywords related to ethnopharmacology, diabetes management, medicinal plants, and dun & duar of Uttarakhand located under shivalik rage of Himalaya (specially Dehradun & Haridwar) were utilized to ensure a thorough search. Although, literatures for above places are merely available in these databases but reviewed plants and herbs are easily cultivated and available in this region and most of these herbs/plants are the part of their diet as seasonal, vegetables and foods. The inclusion criteria for literatures involved a critical review of the identified references to ensure that only high-quality and pertinent studies were incorporated into the review. High blood sugar levels (hyperglycaemia) caused by inefficiency in insulin secretion, action, or both characterize diabetes mellitus or DM, a chronic metabolic disease. DM became one of the most serious, common and life-threatening disease and this is continuously reducing the life expectancy [4]. Type 1 diabetes is an autoimmune disease that results in a lack of insulin when the body’s immune system mistakenly targets and kills the pancreatic cells responsible for making it. Contrarily, insulin resistance, a condition in which the body’s cells become resistant to insulin and the pancreas fails to produce enough insulin to make up for it, is what causes Type 2 diabetes. Increased thirst, frequent urination, blurred vision, exhaustion, and slowly healing wounds are all signs of diabetes [5–7]. Serious complications from uncontrolled diabetes might include kidney failure, cardiovascular disease, neuropathy, and retinopathy etc. [1][8]. Type-II diabetes mellitus (T-II DM) is a growing concern in India and even in worldwide, where sedentary lifestyles, unhealthy eating habits, and genetic predisposition have led to an increase in the incidence of T-II DM [7][8]. Due to their efficiency and lack of adverse effects, plant-based treatments have gained popularity for the treatment of T-II DM last two to three decades. In this article, we’ll provide an overview of the plants that are frequently uses to treat T-II DM. The basic type and causes of diabetes mellitus are represented diagrammatically by figure 1.
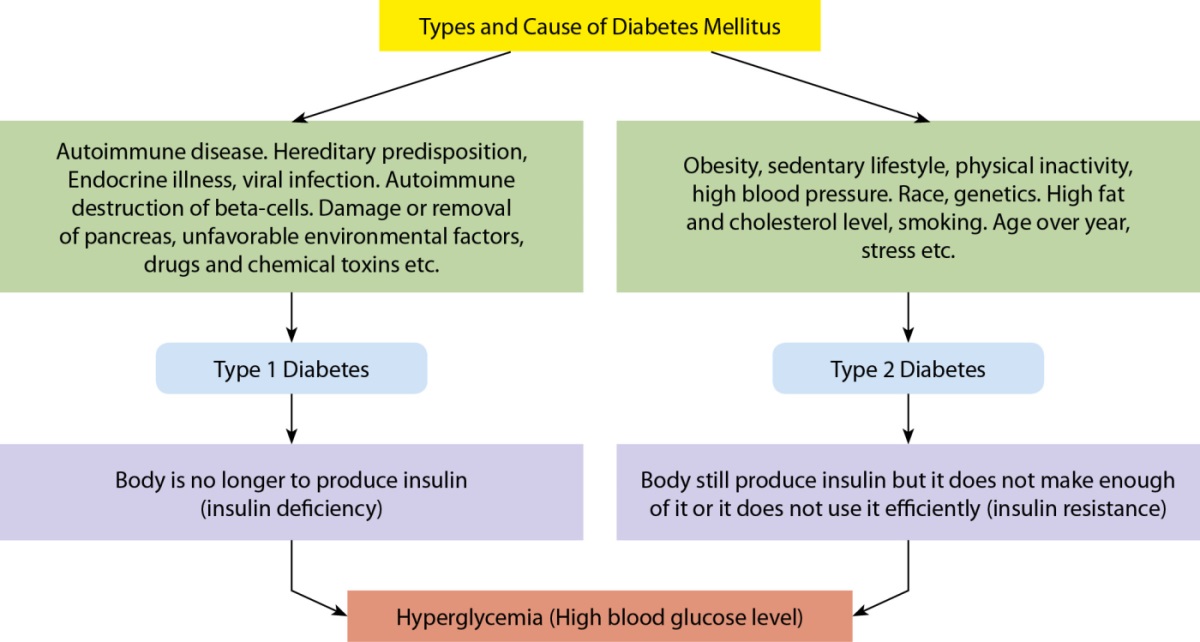
Figure 1. Basic types and Causes of Diabetes mellitus.
The purpose of this review is to shed light on the abundance of ethnopharmacological knowledge that exists in this part of India and explore the possibility of using native medicinal plants to provide complementary or alternative treatments for the management of diabetes. The review’s goal is to expand the knowledge of traditional medicine and its use within contemporary healthcare, especially in combating towards diabetes and its complications, by gathering and assessing these insights.
Pathophysiology of Diabetes Mellitus
Hyperglycaemia, or elevated blood sugar levels, is an indicator of diabetes mellitus, a long-term metabolic condition caused by deficiencies in insulin secretion, activity, or both. An autoimmune process causes the pancreatic beta cells to be destroyed in T-I DM, resulting in an absolute insulin deficiency. In T-II DM, the development of insulin resistance and relative insulin shortage is caused by a confluence of genetic and environmental variables, including as obesity, physical inactivity, and ageing [7][9]. Insulin resistance is the result of reduced glucose absorption and utilisation by target tissues, including muscle, the liver, and adipose tissue. Insulin resistance is brought on by a combination of impaired insulin signalling and post-receptor abnormalities. In response, the pancreas compensates by producing more insulin, which initially maintains normoglycemia but eventually leads to beta cell exhaustion and failure [5]. The hyperglycaemia of diabetes leads to a range of systemic complications affecting various organs and tissues including macrovascular problems like cardiovascular disease, stroke, and peripheral vascular disease as well as microvascular complications like retinopathy, nephropathy, and neuropathy [5][10].
Advanced glycation end products, oxidative stress, inflammation, and altered signalling pathways serve as the underlying mechanisms of these problems, which result in endothelial dysfunction, tissue damage, and organ failure [7]. In conclusion, the pathophysiology of diabetes is complex and multifactorial, involving a range of genetic, environmental, and metabolic factors, as well as intricate interactions between various organs and tissues. Understanding these mechanisms is essential for developing effective prevention and treatment strategies for this growing global health problem. The pathophysiology of diabetes mellitus has been diagrammatically represented by figure 2.
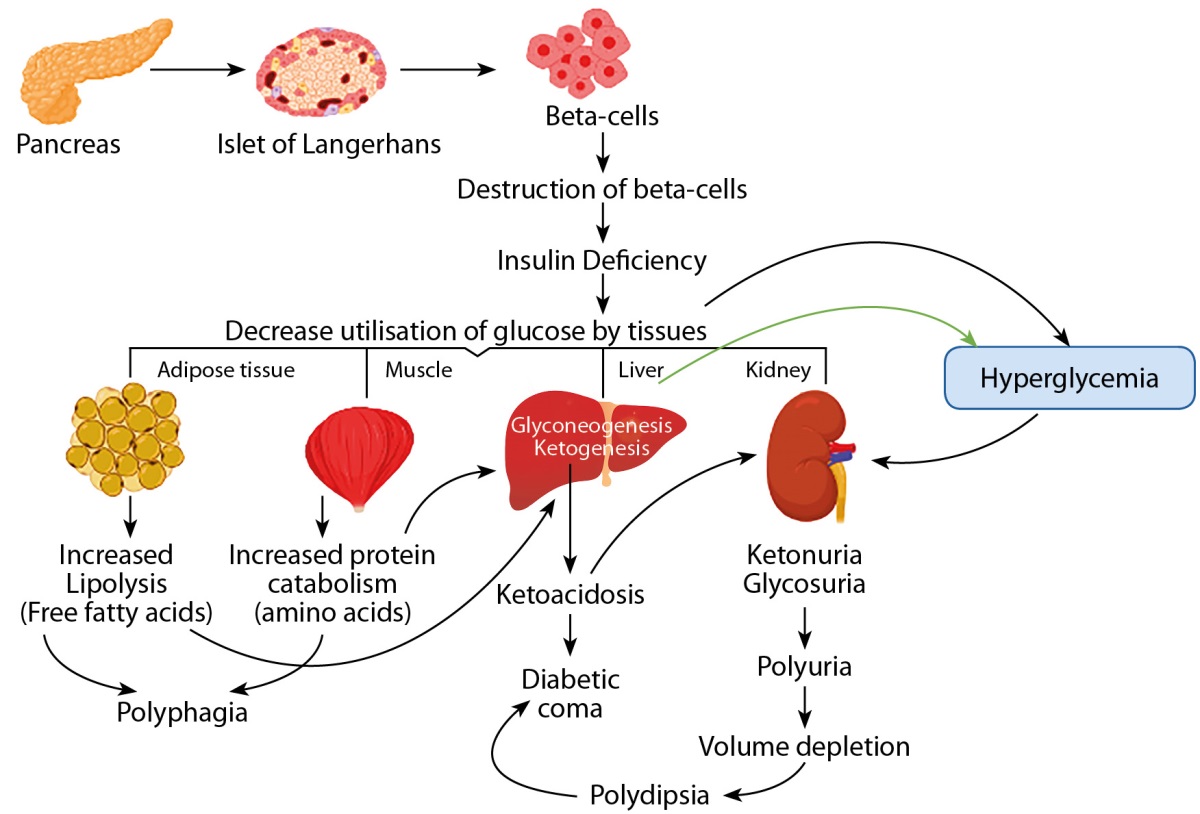
Figure 2. Pathophysiology of Diabetes Mellitus
Summary of Some Medicinal Plants with a Brief Description
1. Syzygium cumini
S. cumini (Myrtaceae) is native to India and commonly known as Jamun and traditionally, it is considered as Holy tree and used as Antidiabetic herbs [11]. Jamun is also used as antihyperlipidemic, antiplaque, neuro-psychopharmacological, nephroprotective, radioprotective, antidiarrheal, antiarthritic, antipyretic, antifertility, antimicrobial, antioxidant, hepatoprotective and antiulcer etc. [12]. The antihyperglycemic potential of S. cumini is supported by a number of research studies. The effectiveness of jamun leaves in preventing «processes of oxidation, glycation, inflammation, and digestive enzyme catalysis» was examined in an investigation published in Journal of Ethnopharmacology. Researchers came to the conclusion that S. cumini had antioxidant and antiglycation features in addition to its capacity for inhibiting digestive enzymes [13]. In another study, investigator used aqueous extract of S. cumini to evaluate its antihyperlipidemic & antidyslipidemic pharmacological potential of it in diabetic rats. After giving 200 mg/kg per day and 400 mg/kg per day for 21 days, they observed a significant decrease in serum insulin levels. Aqueous extract of S. cumini also showed a significant reduction in insulin resistance and improvement in beta-cells` functions [14]. After critically study of many studies, it can be concluded as seeds and leaves of S. cumini have a great antidiabetic potential. Generally, peoples consumed jamun as a fruit and its low toxicity, clinically safe nature and easy availability makes it a prominent antidiabetic herb.
2. Bauhinia variegata
B. variegata (Fabaceae) is distributed all over the India including Uttarakhand and it is popularly called as Kachnar. Numerous phytochemicals, including glycosides, flavonoids, saponins, kaempferol, tannins, and terpenoids, may be found in abundance in each part of this plant, which is why it is so well-known as a medicinal tree. Traditionally, it has been used to cure different diseases like diabetes mellitus, hyperlipidaemia etc. [15]. To confirm its antidiabetic effect, a study was conducted on STZ (streptozotocin) induced diabetic rats by administering ethanolic (EtOH) extract of Kachnar leaf (once daily for 21 days). At the end of study, investigator observed a significant reduction in blood glucose level at 400 mg/kg (highest dose) of EtOH extract of Kachnar leaf. Study also explored its antihyperlipidemic and antioxidant potential [16]. A comparative study between five medicinal plants also enlightened the antidiabetic activity of B. variegata. By doing in vitro evaluation of these five medicinal plants (A. indica/Neem, B. variegata/Kachnar, Dalbergia sissoo/Tahli, Psidium guajava/amrood and S. cumini/Jamun), authors concluded their findings as methanolic leaf extracts of kachnar and jamun exhibit better antidiabetic and antioxidant potential than remaining three medicinal plants [17]. Additionally, Kachnar could potentially induce mild gastric discomfort in individuals with a sensitive stomach. Large doses of Guggul may lead to adverse effects such as headaches, nausea, diarrhoea, hiccups, allergic reactions, skin and itching [15].
3. Aegle marmelos
A. marmelos (Rutaceae) is native to India and easily found in areas focused for review, it is commonly known as Bael which is considered holy by Hindus. Traditionally, its bark, leaves, stem, fruit and seeds have been used as medicinal herbs due to their various pharmacological significances. A. marmelos have antihyperglycemic effect, antiulcer, antidiarrheal, gastroprotective, antiviral, cardioprotective effects etc. [18]. There are a lot of scientific evidences which confirmed the antidiabetic potential of A. cumini. One of them is published in ‘Journal of Food Biochemistry’ and in this, the investigators used leaf extract of A. cumini (Alkaloid free hydroalcoholic) to investigate the antidiabetic potential of Bael. The findings of this study are significantly decreased blood sugar level, ameliorated state of dyslipidaemia, status of oxidative stress in diabetic mice. Even, authors found improved functions of pancreatic beta cells [19]. In a different study, the alcohol-based A. cumini leaf extract’s potential to combat diabetes is investigated. Also, they have conducted its cytotoxicity study in vitro by using HepG2 cells. Finally, they came to the conclusion that A. cumini would be an exceptional restorative therapy for DM and related disorders [20].
4. Azadirachta indica
A. indica (Meliaceae), a plant native to India, is popularly called as nimba or neem in India. It is recognised to have antidiabetic, antipyretic, anti-inflammatory, and antibacterial effects and has a broad range of clinical relevance [21][22]. There are a lot of scientific evidences about antidiabetic potential of Neem and one of them published in Journal of Ayurveda and Integrative Medicine investigated it on high fat diet induced diabetic rats. In this study, after giving diabetic rats 400 mg/kg of A. indica leaf extract for 30 days, researchers noticed the impairment in glucose tolerance, the insulin signalling system, glucose oxidation, and glycogen concentration. At the dose of leaf extract supplied, researchers also observed normalisation in aberrant levels of blood sugar, serum insulin, insulin signalling molecules, and GLUT4 (glucose transporter type-4) proteins. Hence, after evaluating these findings, we can conclude it as A. India exhibit a significant role in the management of T-II DM [23]. In various studies, it has been also observed that A. indica shows dose dependent toxicity on different animal model like mice, rats & hamster etc [24–28]. But mostly it adversely affects liver & kindly as in a study, investigators suggested that due to high concentration of nimbolide and nimbic acid, it causes hepatocyte degeneration [24–26]. Also, it had shown to give rise to skin allergens [25][28].
5. Momordica charantia
M. charantia (Cucurbitaceae) is commonly called as Karela and traditionally, the people of these regions of India used it as an herbal medicine and vegetable. Other names for karela include bitter melon and bitter gourd. Karela has antidiabetic, anti-inflammatory, antibiotic and blood purifying properties. Various scientific studies showed that the fruit and leaves of karela has a great antidiabetic potential [29–32]. The electronic journal of biotechnology recently released a study on how M. charantia saponin (MCS) affected oxidative stress and the insulin signalling system in type II diabetic rats. Additionally, it was observed that MCS might lower fasting blood sugar levels and enhance rats’ glucose tolerance, insulin sensitivity, and insulin content [30]. There are a lot of scientific evidences which provide the clarity about the antidiabetic and hypoglycaemic effects of karela or M. charantia [29]. Numerous toxicological investigations have illustrated those extracts from M. charantia may induce toxicity in various organs at different dosage levels [33–36]. Recently, a zebrafish study confirmed its teratogenic and cardiotoxic effects at specific doses [33]. Additionally, in 2020, Abdillah et al. documented hepatotoxic and nephrotoxic effects of M. charantia ethanolic extract over 28 days [34]. Further clarification of these reported toxicities on vital organs is necessary to establish a safe dosage for usage.
6. Trigonella frenum-graecum
T. frenum-graecum (Fabaceae) is commonly known as Methi or fenugreek and traditionally its seeds and leaves have been commonly used as seasoning and vegetable in all over India. Its seeds have antidiabetic, antihyperlipidemic, antidepressant, antianxiety, antioxidant as well as immunomodulating effects [37]. A randomizes controlled clinical trial study investigated antidiabetic effect of fenugreek on diabetic patients. This study was conducted on 12 uncontrolled diabetic patients where investigator gave 2 gm methi per day to patients. After 12 weeks, investigator noticed a significant increment in fasting insulin level but insignificant reduction in fasting blood sugar level [38]. Another study was published in Journal of Diabetes Research which also investigated the antidiabetic effect of fenugreek seed powder. This study was performed on 114 newly diagnosed diabetic patients and investigator found pronounced effect in lipid metabolism in T-II diabetic patients without any side effects. Hence, it can be concluded as fenugreek may give new alternatives for the clinical management of T-II DM [39]. The potential side effects of methi and its various preparations have been investigated to identify possible adverse reactions. While major clinical trials assessing Trigonella’s use as conventional or alternative herbal medicine are lacking, current knowledge of its side effects primarily stems from user-reported symptoms and animal studies, including stomach upset, diarrhoea, or bloating [40][43]. Also, the intake of fenugreek seeds during pregnancy has been linked to a spectrum of congenital abnormalities, such as hydrocephalus, anencephaly, and spina bifida [41]. The findings of another study, indicate that exposing mice to a high dose of fenugreek seeds during prenatal development led to growth delays and changes in neurobehavioral performance after weaning [42]. However, the underlying molecular mechanisms behind these effects still require further investigation [43].
7. Gymnema sylvestre
Common names for G. sylvestre (Apocynaceae) are Gurmar and madhunashini. Historically, diseases like diabetes, arthritis, dental caries, anaemia, hypercholesterolemia, asthma, constipation, and others have been treated with the seeds and leaves of the Gurmar plant in Dehradun & Haridwar as well as whole Northern region of India. Gurmar has promising diabetes therapeutic potential since it has a favourable impact on blood sugar homeostasis, manages sugar cravings, and encourages pancreatic regeneration [44]. According to a study published in the Journal of Ethnopharmacology, 22 T-II DM patients taking conventional oral antidiabetic medications participated in the trial to determine the efficiency of an extract (GS4) from the leaves of Gurmar in lowering blood sugar levels. For a period of 18 to 20 months, 400 mg of GS4 was given daily as a complement to the usual oral anti-diabetic medications. Patients who underwent this therapy experienced a considerable decrease in their blood sugar levels, glycosylated haemoglobin and plasma proteins, as well as a reduction in the frequency and quantity of their regular antidiabetic medication. Out of the 22 T-II DM patients, 5 were able to discontinue using their traditional medications and maintain blood sugar homeostasis with GS4 alone. The presence of elevated insulin levels in the serum of T-II DM patients supports the assertion that these data also imply that the beta cells of the pancreas may be restored in T-II DM patients with GS4 supplementation [45]. There are not many numbers of literatures which declared G. Sylvester as toxic but, in some studies, its toxicity has been observed. Shiyovich et. al., (2010) reported a case of G. sylvestre induced liver injury (toxic hepatitis) [46] as well as Khare et. al., (1983) observed its hypoglycaemic effect on non-diabetic & diabetic patients [47].
8. Ocimum sanctum
O. tenuiflorum or O. sanctum (Lamiaceae) is native to Indian subcontinent and it can be easily found all over the India [48]. It is basically found in two variant that are Rama Tulsi or Sri Tulsi (green coloured leaves) and Krishna Tulsi (Purple coloured leaves) [49]. It considered as sacred plant by Hindus and it is commonly known as Tulsi or Holy basil. It contains more than 60 phytochemicals including steroids, phenols, phenyl propanoids, essential oils etc. and it is scientifically proven that it is used as antidiabetic, antioxidant, anticancer, antistress and anti-inflammatory etc. [48]. Numerous in vitro, in vivo, and clinical studies have been carried out to check O. sanctum’s antidiabetic efficacy. One of them is published in ‘Caspian journal of Internal medicine’ and in this, investigator used MeOH (methanolic) leaf extract of Tulsi to conduct the evaluation of IVIV (In vitro-In vivo) antidiabetic and antioxidant activity. The STZ-induced diabetic Wistar rat model was chosen by researchers for in vivo research, and suppression both α-amylase and α-glucosidase was used for in vitro research. Finally, researchers reported that diabetic wistar rats had significantly lower blood glucose levels and oxidative stress [50]. Three species of tulsi (O. basilicum L./Green Tulsi, O. gratissimum L./Jungli Tulsi, and O. tenuiflorum/Black Tulsi) have been found to have considerable anti-inflammatory and anti-diabetic potential in a comparative research [51]. Although tulsi is very spiritual plant in Sanatan Dharma and many peoples administering it on daily basis as herb for all diseases, but it can be toxic for any individuals as it can give rise to skin allergens as well as it is contraindicated with anticoagulants and antiplatelets drugs [52][53].
9. Tinospora cordifolia
T. cordifolia (Menispermaceae) is a native to India and traditionally, peoples used it as a medicinal plant. Giloy (T. cordifolia) exhibits antidiabetic, gastroprotective, antidiarrheal, anti-inflammatory, antioxidant and analgesic properties. Even many people believed that it has great potential in the treatment of typhoid, dengue and malarial fever as well as people used to drink its juice as an immunostimulant drink [54]. A scientific study regarding antidiabetic potential of Guduchi/Giloy has been published in Innovative food science and emerging technology states that phytochemicals of T. cordifolia have similar effect as insulin and antihyperglycemic property. And authors found that chloroform extract of Giloy shown highest hypoglycaemic activity as IC50-11.34mg/ml. There is an issue regarding its low bioavailability and poor stability which limits its antidiabetic potential but author used whey protein-based electro sprayed nanospheres and observed a tremendous increment (28.12%) in its activity. By using modern drug delivery systems as nanospheres, liposomes, neosomes, nanobubbles, nano diamonds etc., we can bypass its low bioavailability and low stability issues. After studying various research and review articles, we can conclude it as T. cordifolia has excellent hypoglycaemic potential and it can provide insulin mimicking effects [54–57]. Giloy is widely regarded as a safe botanical entity, with scant scientific literature documenting any potential toxicity. In a study conducted by Gupta & Sharma (2003) have shown that administering a 70% methanolic extract of Tinospora cordifolia stem orally can result in reduced sperm motility and density, decreased serum testosterone levels, as well as lowered protein, sialic acid, and glycogen contents. Additionally, this extract has been found to deplete vesicular fructose in the testes, ultimately leading to diminished male fertility in rat subjects [58].
10. Allium sativum
A. Sativum (Amaryllidaceae), a flowering plant is widely used for flavouring and seasoning purpose. There is a lot of human and animal studies which confirms that garlic has copious number of medicinal properties due to its sulphur containing phytochemicals. It shows antidiabetic effect, cardioprotective property, antimicrobial effect, anticancer, antioxidants and hypoglycaemic effects etc. Since last two decades, garlic became popular for its antidiabetic effect [59][60]. In an investigation, authors compared antidiabetic effect of Garlic with glibenclamide (600 microgram/kg). Author gave garlic extract for 14 days via oral route to normal and STZ-induced rats and evaluated its effect on level of glucose, triglycerides, total cholesterol, AST and ALT. Investigator observed significant decrease in level of glucose, urea, uric acid, AST, creatinine, total cholesterol, triglyceride and concluded the study as garlic extract exhibit better antidiabetic effect than glibenclamide [61]. There are lot of scientific evidences published in various reputed international journals and reports that support the hypoglycaemic property of garlic [59–64]. Generally, garlic is used as a part of diet worldwide and its low toxicity, clinically safe and cost-effectiveness make it first choice as a complete solution for many ailments.
DISCUSSION & CONCLUSION
As it is already discussed that shivalik range of Himalaya (specially Dehradun & Haridwar) of Uttarakhand, India is highly rich in biodiversity of medicinal plants. Since thousands of years, these are used by local population to get relief from various diseases including diabetes. Various scientific studies have been cited in this review which confirms that these medicinal plants are the best alternative to allopathic medicines to treat or even cure the diabetes mellitus. These medicinal herbs have the potential to control the blood glucose level as well as increase the blood insulin level and repair the insulin secretory cells of pancreas. Botanical source, vernacular names and possible clinical significance of these medicinal plants are shown in table 1. All the findings of this review suggests that individual plant mentioned above is capable to treat diabetes and if they are taken along with any medicines like metformin, glibenclamide etc., they show synergistic action on the diabetes mellitus and enhance the efficacy of that particular medicine. These all herbs like Giloy, Jamun, Neem, Methi, Karela, Gurmar, Lehsun etc. are easily found in whole northern region of India including Dehradun & Haridwar and local peoples of this region used these plants or herbs directly or indirectly to treat diabetes since thousands of years. Most of these discussed plants are used as vegetables, seasoning, flavouring and spices etc. Complications of diabetes mellitus result not only from high blood glucose and there are some other serious complications associated with diabetes like kidney failure, impairment in glucose tolerance, insulin signalling system, insulin sensitivity, glucose oxidation, and glycogen concentration, oxidative stress, obesity, liver dysfunction etc. Many literatures suggest that the people living with their traditional lifestyle are maintaining their fitness and health by using these traditional plants as a part of their diet but since last two or three decades, modernisation and urbanisation drastically affects their lifestyle and food patterns. This sedentary lifestyles, unhealthy eating habits, and genetic predisposition played a vital role in increment in the cases of diabetes mellitus in this region [116][117]. With phytotherapy, there is a problem of their less bioavailability and rate of absorption. As compare to allopathic therapy, phytotherapy shows less potency and efficacy towards its targeted site and disease. But in the field of pharmaceutics, there are various advanced dosage forms (phytosomes, neosomes, liposomes, nanoparticles, nanobubbles, nano diamonds, microsphere etc.) and method of delivery (various invasive and non-invasive methods) which can bypass these all problems associated with the potency and efficacy of phytochemicals [118–120]. Various superdisintegrants, advanced polymers and other excipients are available in the market which have capability to increase their bioavailability, rate of absorption, retention time, contact time, rate of dissolution and disintegration etc. Although phytotherapy has very less toxic effect, but various toxicological evidences also confirm it that these herbs or plants can be a greater alternate to the existing medicines [121][122]. If we see the trend, most of the researcher related to pharmacy field are doing investigation on phytochemicals and exploring their clinical significances. These all efforts indicate that phytotherapy has an excellent potential to treat or even cure these deadly diseases including diabetes mellitus. After reviewing many research and review articles, we can conclude it as mentioned plants or herbs have a great potential to prevent, treat and cure diabetes mellitus.
Table 1. List of traditional plants used to treat Diabetes Mellitus type 2.
|
S. No. |
Botanical Name |
Family |
Vernacular name |
Part used |
Ethnopharmacological uses |
Reference |
|
1 |
Gymnema sylvestre |
Apocynaceae |
Gurmar, Madhunashini |
Seed, Leaves |
Antidiabetic, Antiarthritic, Dental carries, Antibiotic, Antimicrobial, Anti-inflammatory, Anticancer, Immunomodulator etc. |
[31][32] |
|
2 |
Momordica charantia |
Cucurbitaceae |
Karela, Bitter melon |
Seeds, Fruit |
Antidiabetic, Anti-inflammatory, Antibiotic etc. |
[24–27][43] |
|
3 |
Azadirachta indica |
Meliaceae |
Neem, Nimba |
Seed, Leaves and Fruit |
Antidiabetic, Antioxidants, Anti-inflammatory, Anticancer effects etc. |
[21][22] |
|
4 |
Trigonella frenum-graecum |
Fabaceae |
Methi, Fenugreek |
Seed, Leaves |
Antidiabetic, Anti-hyperlipidemia, Antioxidants, neurological disorders etc. |
[28][30] |
|
5 |
Syzygium cumini |
Myrtaceae |
Jamun, Jambul |
Seed, Fruit |
Antidiabetic, Antihyperlipidemic, Antiulcer, Hepatoprotective, Antiplaque, Antipyretic, Antidiarrheal etc. |
[11][12] |
|
6 |
Terminalia chebula |
Combretaceae |
Harad, Haritaki |
Fruit, Bark |
Antidiabetic, Gastroprotective, Antiparasitic, Hepatoprotective, Antioxidant, Antiaging etc. |
[47][48] |
|
7 |
Berberis aristate |
Berberidaceae |
Daru Haldhi, Daruharidra, Zarishk |
Leaves, Wood |
Antidiabetic, Cardiovascular complications, Oxidative stress, neurodegeneration, hepatic dysfunctions etc. |
[32][49] |
|
8 |
Allium sativum |
Amaryllidaceae |
Lehsun, Garlic |
Bulb, Leave |
Antidiabetic, Cardiovascular diseases, common cold, cancer, Antimicrobial, Antiviral etc. |
[50][51] |
|
9 |
Aegle marmelos |
Rutaceae |
Bael,Bilva, Wood Apple |
Fruit, Leaves |
Antidiabetic, Gastroprotective, Antidiarrheal, Radioprotective, Cardioprotective, Antimicrobial etc. |
[52][53] |
|
10 |
Nardostachys jatamansi |
Caprifoliaceae |
Jatamansi, Muskroot |
Whole Plant |
Antidiabetic, Hepatoprotective, Anti-Parkinson, Hypoglycemic insecticidal, Anticancer, Anticonvulsant etc. |
[54][55] |
|
11 |
Acacia catechu |
Fabaceae |
Katha, Khadir |
Bark, Wood, Seed |
Antidiabetic, Strong Antioxidant, Astringent, Antimicrobial, Immunomodulatory etc. |
[56][57] |
|
12 |
Bauhinia variegata |
Fabaceae |
Kachnaar, Orchid tree |
Flower |
Antidiabetic, Antihyperlipidemic, Antioxidant |
[15][16] |
|
13 |
Piper longum |
Piperaceae |
Pippalli |
Fruit, Leaves, Root |
Antidiabetic, Immunomodulatory, Insomnia, Dementia, Epilepsy Carminative etc. |
[58–60] |
|
14 |
Ocimum sanctum |
Lamiaceae |
Tulsi, Holy basil |
Leaves, Wood |
Antidiabetic, Antistress, Radioprotective, Anticough, leishmanicidal, Antioxidant, Anti-inflammatory etc. |
[33][61] |
|
15 |
Andrographis paniculate |
Acanthaceae |
Kalmegh, King of Bitter |
Leaves, Root |
Antidiabetic, Antiviral, Jaundice, Anti-obesity, Anti-inflammatory, Anticancer etc. |
[62][63] |
|
16 |
Pterocarpus marsupium |
Faboideae |
Vijaysar, Indian Kino |
Heart Wood, Seeds |
Antidiabetic, Analgesic, Anti-inflammatory, Hepatoprotective, Antifungal, Antioxidants etc. |
[64][65] |
|
17 |
Commiphora wightii |
Burseraceae |
Guggul, Indian bdellium tree |
Resin, Fruit |
Antidiabetic, Cardioprotective, IBD, Ulcer, Arthritis etc. |
[66–68] |
|
18 |
Boerhaavia diffusa |
Nyctaginaceae |
Punarnava |
Leaves, Flowers, Pollen |
Antidiabetic, Anemia, Oedema, Expectorants, R.A., Anticonvulsants etc. |
[69][70] |
|
19 |
Casearia esculenta |
Salicaceae |
Saptarangi |
Root |
Antidiabetic, Antihyperlipidemic, Anticaries activity, RFA, Hepatoprotective etc. |
[71–73] |
|
20 |
Swertia chirata |
Gentianaceae |
Chirayata |
Whole plant |
Antidiabetic, Bitter tonic, febrifuge, Antiperiodic, stomachic etc. |
[74–76] |
|
21 |
Tinospora cordifolia |
Menispermaceae |
Giloy, Guduchi |
Leaves, Fruits |
Antidiabetic, Antioxidant, Immunomodulatory, Anti-inflammatory, Anticancer etc. |
[37][38][41][42][77] |
|
22 |
Lepidium sativum |
Brassicaceae |
Chandraprabha, Haloon |
Seed, Sprouts |
Antidiabetic, Antidiarrheal, Antioxidant, Antiasthmatic, Bone fracture etc. |
[78][79] |
|
23 |
Phyllanthus emblica |
Phyllanthaceae |
Amla |
Fruits |
Antidiabetic, Antiviral, Antifungal, Antiallergic, Antimicrobial etc. |
[80][81] |
|
24 |
Picrorhiza kurroa |
Plantaginaceae |
Kutki |
Leaves, Flower, Rhizome |
Antidiabetic, Cardioprotective, Antimalarial, Immunomodulatory, Antimicrobial etc. |
[82][83] |
|
25 |
Cassia fistula |
Fabaceae |
Amaltas |
Stem Bark, Seed, Leaves |
Antidiabetic, Antioxidant, Hepatoprotective, Antitumor, Antimicrobial, Anti-inflammatory etc. |
[84–86] |
|
26 |
Butea monosperma |
Fabaceae |
Palash |
Flowers |
Antidiabetic, Antioxidant, Anti-inflammatory, matrix metalloproteinase inhibitory activities etc. |
[87][88] |
|
27 |
Tribulus terrestris |
Zygophyllaceae |
Gokharu |
Fruits, Burs |
Antidiabetic, Antiurolithic, Anthelminthic, Antispasmodic, Anticariogenic activities etc. |
[89][90] |
|
28 |
Crocus sativus |
Iridaceae |
Kesar, Saffron |
Stigmas, Flower |
Antidiabetic, pleotropic anti-inflammatory effects, neuroprotective, Antioxidants etc. |
[91][92] |
|
29 |
Zingiber officinale |
Zingiberaceae |
Adrak, Ginger |
Rhizome |
Antidiabetic, Anticlotting, Anti-inflammatory, Analgesic etc. |
[93–95] |
|
30 |
Withania somnifera |
Solanaceae |
Ashwagandha, Indian Ginseng |
Leaves, Root |
Antidiabetic, Antihyperlipidemic, Oxidative stress, Immunomodulator etc. |
[96][97] |
Abbreviations. DM: diabetes mellitus, RA: rheumatoid arthritis, IBD: inflammatory bowel disease, RFA: reproductive function activity, AST: aspartate aminotransferase, ALT: alanine aminotransferase
ABBREVIATIONS
DM: diabetes mellitus, T-I: type-I, T-II: type-II, WHO: world health organisation, IDF: international diabetes federation, STZ: streptozotocin, EtOH: ethanol, MeOH: methanol, RA: rheumatoid arthritis, IBD: inflammatory bowel disease, RFA: reproductive function activity, HepG2: human liver cancer cell line, GLUT-4: glucose transporter type-4, MCS: Momordica charantia saponin, GS4: Gymnema sylvestre extract, IVIV: In-vitro In-vivo, AST: aspartate aminotransferase, ALT: alanine aminotransferase.
ADDITIONAL INFORMATION
Participation of authors. Sachin Kumar – conceptualization, writing, original draft preparation; Ashok Kumar – supervision, study design; Junaid Tantray – literature survey, editing; Aman Shukla – writing, reviewing and editing.
Declaration of conflicting interests: The authors declare no conflict of interest.
Acknowledgements: The authors are thankful to their parents and the Dean and Director, School of Pharmacy, Graphic Era Hill University, Dehradun for providing support, guidance and valuable data.
Funding: Nil
References
1. WHO. (2023). Diabetes. World Health Organisation. https://www.who.int/health-topics/diabetes
2. Knwal, S. Diabetes in India-statistics & facts. Health,Pharma and Medtech. Sanyukta Kanwal. Retrieved February 7, 2023, https://www.statista.com/topics/10473/diabetes-in-india/
3. Sun H, Saeedi P, Karuranga S, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Research And Clinical Practice. 2022;183:109119. https://doi.org/10.1016/j.diabres.2021.109119
4. Magliano DJ, Chen L, Islam RM, et al. Trends in the incidence of diagnosed diabetes: a multicountry analysis of aggregate data from 22 million diagnoses in high-income and middle-income settings. The Lancet Diabetes & Endocrinology. 2021;9(4):203-11. https://doi.org/10.1016/S2213-8587(20)30402-2
5. Patton KT, Thibodeau GA. Anthony’s Textbook of Anatomy & Physiology-E-Book. Elsevier Health Sciences; 2018 Mar 5. https://shop.elsevier.com/books/anthonys-textbook-of-anatomy-and-physiology/patton/978-0-323-52880-1
6. Joshua SR, Shin S, Lee JH, Kim SK. Health to Eat: A Smart Plate with Food Recognition, Classification, and Weight Measurement for Type-2 Diabetic Mellitus Patients’ Nutrition Control. Sensors. 2023;23(3):1656. https://doi.org/10.3390/s23031656
7. Banasik JL. Pathophysiology-E-Book. Elsevier Health Sciences; 2021 May 29. https://books.google.com/books/about/Pathophysiology_E_Book.html?id=2ZgwEAAAQBAJ
8. Shojima N, Yamauchi T. Progress in genetics of type 2 diabetes and diabetic complications. Journal Of Diabetes Investigation. 2023;14(4):503-15. https://doi.org/10.1111/jdi.13970
9. Hinault C, Caroli-Bosc P, Bost F, Chevalier N. Critical overview on endocrine disruptors in diabetes mellitus. International Journal Of Molecular Sciences. 2023;24(5):4537. https://doi.org/10.3390/ijms24054537
10. Desai A, Chen R, Cayetano A, et al. Understanding and treating ejaculatory dysfunction in men with diabetes mellitus. Andrology. 2023;11(2):379-98. https://doi.org/10.1111/andr.13262
11. Jagetia GC. Antidiabetogenic action of jamun Syzygium cumini Skeels: a review. Int J Complement Alt Med. 2023;16(2):88-97. https://doi.org/10.15406/ijcam.2023.16.00636
12. Srivastava S, Chandra D. Pharmacological potentials of Syzygium cumini: a review. Journal Of The Science Of Food And Agriculture. 2013;93(9):2084-93. https://doi.org/10.1002/jsfa.6111
13. Franco RR, Zabisky LF, de Lima Júnior JP, et al. Antidiabetic effects of Syzygium cumini leaves: A non-hemolytic plant with potential against process of oxidation, glycation, inflammation and digestive enzymes catalysis. Journal Of Ethnopharmacology. 2020; 261:113132. https://doi.org/10.1016/j.jep.2020.113132
14. Sharma S, Pathak S, Gupta G, et al. Pharmacological evaluation of aqueous extract of syzigium cumini for its antihyperglycemic and antidyslipidemic properties in diabetic rats fed a high cholesterol diet—Role of PPARγ and PPARα. Biomedicine & Pharmacotherapy. 2017; 89:447-53. https://doi.org/10.1016/j.biopha.2017.02.048
15. Sharma K, Kumar V, Kumar S, et al. Bauhinia variegata: a comprehensive review on bioactive compounds, health benefits and utilization. Advances In Traditional Medicine. 2021; 21:645-53. https://doi.org/10.1007/s13596-020-00472-4
16. Tripathi AK, Gupta PS, Singh SK. Antidiabetic, anti-hyperlipidemic and antioxidant activities of Bauhinia variegata flower extract. Biocatalysis And Agricultural Biotechnology. 2019; 19:101142. https://doi.org/10.1016/j.bcab.2019.101142
17. Bakshi A, Sharma N, Nagpal AK. Comparative evaluation of in vitro antioxidant and antidiabetic potential of five ethnomedicinal plant species from Punjab, India. South African Journal Of Botany. 2022;150: 478-87.https://doi.org/10.1016/j.sajb.2022.08.019
18. Chanda R, Ghosh A, Mitra T, et al. Phytochemical and pharmacological activity of Aegle marmelos as a potential medicinal plant: An overview. The Internet Journal Of Pharmacology. 2008;6(1):3. https://doi.org/10.1016/j.joim.2018.04.007
19. Ibrahim M, Parveen B, Zahiruddin S, et al. Analysis of polyphenols in Aegle marmelos leaf and ameliorative efficacy against diabetic mice through restoration of antioxidant and anti‐inflammatory status. Journal Of Food Biochemistry. 2022;46(4):e13852. https://doi.org/10.1111/jfbc.13852
20. Ahmad W, Amir M, Ahmad A, et al. Aegle marmelos leaf extract phytochemical analysis, cytotoxicity, in vitro antioxidant and antidiabetic activities. Plants. 2021;10(12):2573. https://doi.org/10.3390/plants10122573
21. Islas JF, Acosta E, Zuca G, et al. An overview of Neem (Azadirachta indica) and its potential impact on health. Journal Of Functional Foods. 2020; 74:104171. https://doi.org/10.1016/j.jff.2020.104171
22. Patil SM, Shirahatti PS, Ramu R. Azadirachta indica A. Juss (neem) against diabetes mellitus: A critical review on its phytochemistry, pharmacology, and toxicology. Journal Of Pharmacy And Pharmacology. 2022;74(5):681-710. https://doi.org/10.1093/jpp/rgab098
23. Satyanarayana K, Sravanthi K, Shaker IA, Ponnulakshmi R. Molecular approach to identify antidiabetic potential of Azadirachta indica. Journal Of Ayurveda And Integrative Medicine. 2015;6(3):165. https://doi.org/10.4103/0975-9476.157950
24. Islas JF, Acosta E, Zuca G, et al. An overview of Neem (Azadirachta indica) and its potential impact on health. Journal Of Functional Foods. 2020;74:104171
25. Patel SM, Nagulapalli Venkata KC, Bhattacharyya P, Sethi G, Bishayee A. Potential of neem (Azadirachta indica L.) for prevention and treatment of oncologic diseases. Semin Cancer Biol. 2016;40-41:100-115. https://doi.org/10.1016/j.semcancer.2016.03.002
26. Lisanti E, Sajuthi D, Agil M, et al. The effect of aqueous seed extract of neem (Azadirachta indica A. Juss) on liver histology of male mice (Mus musculus albinus). AIP Conf. Proc. 10 October 2018; 2019;(1):060004. https://doi.org/10.1063/1.5061913
27. Batista FLA, Lima LMG, Abrante IA, et al. Antinociceptive activity of ethanolic extract of Azadirachta indica A. Juss (Neem, Meliaceae) fruit through opioid, glutamatergic and acid-sensitive ion pathways in adult zebrafish (Danio rerio). Biomed Pharmacother. 2018;108:408-416. https://doi.org/10.1016/j.biopha.2018.08.160
28. Deng YX, Cao M, Shi DX, et al. Toxicological evaluation of neem (Azadirachta indica) oil: acute and subacute toxicity. Environ Toxicol Pharmacol. 2013;35(2):240-246. https://doi.org/10.1016/j.etap.2012.12.015
29. Joseph B, Jini D. Antidiabetic effects of Momordica charantia (bitter melon) and its medicinal potency. Asian Pacific Journal Of Tropical Disease. 2013;3(2):93-102. https://doi.org/10.1016/S2222-1808(13)60052-3
30. Jiang S, Xu L, Xu Y, et al. Antidiabetic effect of Momordica charantia saponins in rats induced by high-fat diet combined with STZ. Electronic Journal Of Biotechnology. 2020;43:41-7. https://doi.org/10.1016/j.ejbt.2019.12.001
31. Richter E, Geetha T, Burnett D, Broderick TL, Babu JR. The Effects of Momordica charantia on Type 2 Diabetes Mellitus and Alzheimer’s Disease. Int J Mol Sci. 2023;24(5):4643. https://doi.org/10.3390/ijms24054643
32. Yedjou CG, Grigsby J, Mbemi A, et al. The Management of Diabetes Mellitus Using Medicinal Plants and Vitamins. Int J Mol Sci. 2023;24(10):9085. Published 2023 May 22. https://doi.org/10.3390/ijms24109085
33. Khan MF, Abutaha N, Nasr FA, Alqahtani AS, Noman OM, Wadaan MAM. Bitter gourd (Momordica charantia) possess developmental toxicity as revealed by screening the seeds and fruit extracts in zebrafish embryos. BMC Complement Altern Med. 2019;19(1):184. https://doi.org/10.1186/s12906-019-2599-0
34. Abdillah S, Inayah B, Febrianti AB, Nafisa S. Acute and Subchronic Toxicity of Momordica Charantia L Fruits Ethanolic Extract in Liver and Kidney. Systematic Reviews in Pharmacy. 2020;11(12):2249-2255
35. Grandjean P. Paracelsus Revisited: The Dose Concept in a Complex World. Basic Clin Pharmacol Toxicol. 2016;119(2):126-132. https://doi.org/10.1111/bcpt.12622
36. Oyelere SF, Ajayi OH, Ayoade TE, et al. A detailed review on the phytochemical profiles and anti-diabetic mechanisms of Momordicacharantia [published correction appears in Heliyon. 2023 Nov 02;9(11):e22019. doi: 10.1016/j.heliyon.2023.e22019]. Heliyon. 2022;8(4):e09253. https://doi.org/10.1016/j.heliyon.2022.e09253
37. Zameer S, Najmi AK, Vohora D, Akhtar M. A review on therapeutic potentials of Trigonella foenum graecum (fenugreek) and its chemical constituents in neurological disorders: Complementary roles to its hypolipidemic, hypoglycemic, and antioxidant potential. Nutritional Neuroscience. 2018;21(8):539-45. https://doi.org/10.1080/1028415X.2017.1327200
38. Najdi RA, Hagras MM, Kamel FO, Magadmi RM. A randomized controlled clinical trial evaluating the effect of Trigonella foenum-graecum (fenugreek) versus glibenclamide in patients with diabetes. African Health Sciences. 2019;19(1):1594-601. https://doi.org/10.4314/ahs.v19i1.34
39. Geberemeskel GA, Debebe YG, Nguse NA. Antidiabetic effect of fenugreek seed powder solution (Trigonella foenum-graecum L.) on hyperlipidemia in diabetic patients. Journal Of Diabetes Research. 2019;2019. https://doi.org/10.1155/2019/8507453
40. Muraki E, Hayashi Y, Chiba H, et al. Dose-dependent effects, safety and tolerability of fenugreek in diet-induced metabolic disorders in rats. Lipids in Health and Disease. 2011;10:1-6. https://doi.org/10.1186%2F1476-511X-10-240
41. Khalki L, M’hamed SB, Bennis M, Chait A, Sokar Z. Evaluation of the developmental toxicity of the aqueous extract from Trigonella foenum-graecum (L.) in mice. J Ethnopharmacol. 2010;131(2):321-325. https://doi.org/10.1016/j.jep.2010.06.033
42. Khalki L, Bennis M, Sokar Z, Ba-M’hamed S. The developmental neurobehavioral effects of fenugreek seeds on prenatally exposed mice. J Ethnopharmacol. 2012;139(2):672-677. https://doi.org/10.1016/j.jep.2011.12.011
43. Yadav UC, Baquer NZ. Pharmacological effects of Trigonella foenum-graecum L. in health and disease. Pharm Biol. 2014;52(2):243-254. https://doi.org/10.3109/13880209.2013.826247
44. Tiwari P, Mishra BN, Sangwan NS. Phytochemical and pharmacological properties of Gymnema sylvestre: an important medicinal plant. BioMed Research International. 2014; 2014:830285. https://doi.org/10.1155/2014/830285
45. Baskaran K, Ahamath BK, Shanmugasundaram KR, Shanmugasundaram ER. Antidiabetic effect of a leaf extract from Gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. Journal Of Ethnopharmacology. 1990;30(3):295-305. https://doi.org/10.1016/0378-8741(90)90108-6
46. Shiyovich A, Nesher L, Sztarkier I. Toxic hepatitis induced by Gymnema sylvestre, a natural remedy for type 2 diabetes mellitus. The American Journal Of The Medical Sciences. 2010 Dec 1;340(6):514-7
47. Khare AK, Tondon RN, Tewari JP. Hypoglycaemic activity of an indigenous drug (Gymnema sylvestre,’Gurmar’) in normal and diabetic persons. Indian J Physiol Pharmacol. 1983;27(3):257-258.
48. Singh D, Chaudhuri PK. A review on phytochemical and pharmacological properties of Holy basil (Ocimum sanctum L.). Industrial Crops and Products. 2018; 118:367-82. https://doi.org/10.1016/j.indcrop.2018.03.048
49. Parajuli-Baral K. Formulation and Evaluation of Quality Parameters of Effervescent Granules from the Potent Antioxidant between Two Variants of the Adaptogenic Herb Ocimum tenuiflorum L. The Scientific World Journal. 2023;2023. https://doi.org/10.1155/2023/2050846
50. Ononamadu CJ, Alhassan AJ, Imam AA, et al. In vitro and in vivo anti-diabetic and anti-oxidant activities of methanolic leaf extracts of Ocimum canum. Caspian Journal Of Internal Medicine. 2019;10(2):162. https://doi.org/10.22088/cjim.10.2.162.
51. Sharma AD, Kaur I, Angish S, et al. Comparative phytochemistry, antioxidant, antidiabetic, and anti-inflammatory activities of traditionally used Ocimum basilicum L. Ocimum gratissimum L., and Ocimum tenuiflorum L. BioTechnologia. 2022;103(2):131. https://doi.org/10.5114/bta.2022.116206
52. Cohen MM. Tulsi-Ocimum sanctum: A herb for all reasons. Journal Of Ayurveda And Integrative Medicine. 2014;5(4):251. https://doi.org/10.4103%2F0975-9476.146554
53. Thakur Ashish. 28. Holy Basil (Ocimum Sanctum)- A Comprehensive Review of Traditional Uses, Phytochemical Composition, Medicinal Properties and Future Directions. The Journal of Agricultural Education and Extension. 3. 136-151.
54. Arunachalam K, Yang X, San TT. Tinospora cordifolia (Willd.) Miers: Protection mechanisms and strategies against oxidative stress-related diseases. Journal of Ethnopharmacology. 2022; 283:114540. https://doi.org/10.1016/j.jep.2021.114540
55. Jain A, Dasgupta N, Ranjan S, et al. Whey protein based electrosprayed nanospheres for encapsulation and controlled release of bioactive compounds from Tinospora cordifolia extract. Innovative Food Science & Emerging Technologies. 2021;69:102671. https://doi.org/10.1016/j.ifset.2021.102671
56. Jain A, Chhajed M, Saluja MS, et al. Treatment of Diabetes with Indian Herbs and Herbal Medicines: A Review. International Journal of Pharmacy & Life Sciences, 14(3). Available at: https://search.ebscohost.com/login.aspx?direct=true&db=afh&AN=164596463&site=ehost-live
57. Kumari A. Ayurvedic Treatment and Home Remedies for Type-2 Diabetes Mellitus. Socio-Scientific Interaction in Diabetes and Cancer and Its Management, 416. https://doi.org/10.9734/bpi/mono/978-81-968135-7-4/CH31
58. Gupta RS, Sharma A. Antifertility effect of Tinospora cordifolia (Willd.) stem extract in male rats. Indian J Exp Biol. 2003 Aug;41(8):885-9.
59. Sanie-Jahromi F, Zia Z, Afarid M. A review on the effect of garlic on diabetes, BDNF, and VEGF as a potential treatment for diabetic retinopathy. Chinese Medicine. 2023;18(1):18. https://doi.org/10.1186/s13020-023-00725-
60. Eidi A, Eidi M, Esmaeili E. Antidiabetic effect of garlic (Allium sativum L.) in normal and streptozotocin-induced diabetic rats. Phytomedicine. 2006;13(9-10):624-9. https://doi.org/10.1016/j.phymed.2005.09.010
61. Çiçek SS. Momordica charantia L.—Diabetes-related bioactivities, quality control, and safety considerations. Frontiers in Pharmacology. 2022; 13:904643. https://doi.org/10.3389/fphar.2022.904643
62. Al-Snafi AE. Medicinal plants with hypoglycemic effect: A review. GSC Biological and Pharmaceutical Sciences. 2023;24(1):147-173. https://doi.org/10.30574/gscbps.2023.24.1.0274
63. Okoro BC, Dokunmu TM, Okafor E, et al. The ethnobotanical, bioactive compounds, pharmacological activities and toxicological evaluation of garlic (Allium sativum): A review. Pharmacological Research-Modern Chinese Medicine. 2023;8. https://doi.org/10.1016/j.prmcm.2023.100273
64. Ozma MA, Abbasi A, Ahangarzadeh Rezaee M, et al. A critical review on the nutritional and medicinal profiles of garlic’s (Allium sativum L.) bioactive compounds. Food Reviews International. 2022;39(9):6324-6361. doi: 10.1080/87559129.2022.2100417
65. Kim HL, Choi BK, Yang SH. Terminalia chebula Medicinal Uses: A Review of in vitro and in vivo Studies. Biotechnology and Bioprocess Engineering. 2022;27(5):729-39. https://doi.org/10.1007/s12257-022-0090-0
66. Wikipedia. Terminalia chebula. Available at: https://en.wikipedia.org/w/index.php?title=Terminalia_chebula&oldid=1149490400
67. Jahan F, Alvi SS, Islam MH. Berberis aristata and its secondary metabolites: Insights into nutraceutical and therapeutical applications. Pharmacological Research-Modern Chinese Medicine. 2022;5. https://doi.org/10.1016/j.prmcm.2022.100184
68. Saikat AS, Hossain R, Mina FB, et al. Antidiabetic effect of garlic. Revista Brasileira de Farmacognosia. 2021;32:1-11. https://doi.org/10.1007/s43450-021-00193-y
69. Gupta RC, Chang D, Nammi S, et al. Interactions between antidiabetic drugs and herbs: an overview of mechanisms of action and clinical implications. Diabetology & Metabolic Syndrome. 2017;9(1):1-2. https://doi.org/10.1186/s13098-017-0254-9
70. Sharma P, Joshi T, Mathpal S, et al. In silico identification of antidiabetic target for phytochemicals of A. marmelos and mechanistic insights by molecular dynamics simulations. Journal Of Biomolecular Structure And Dynamics. 2022;40(21):10543-60. https://doi.org/10.1080/07391102.2021.1944910
71. Manandhar B, Paudel KR, Sharma B, Karki R. Phytochemical profile and pharmacological activity of Aegle marmelos Linn. Journal Of Integrative Medicine. 2018;16(3):153-63. https://doi.org/10.1016/j.joim.2018.04.007
72. Song MY, Bae UJ, Lee BH, et al. Nardostachys jatamansi extract protects against cytokine-induced β-cell damage and streptozotocin-induced diabetes. World Journal Of Gastroenterology. 2010;16(26):3249. https://doi.org/10.3748/wjg.v16.i26.3249
73. Kaur H, Lekhak MM, Chahal S, et al. Nardostachys jatamansi (D. Don) DC.: An invaluable and constantly dwindling resource of the Himalayas. South African Journal Of Botany. 2020;135:252-67. https://doi.org/10.1016/j.sajb.2020.08.010
74. Aryal B, Adhikari B, Aryal N, et al. LC-HRMS profiling and antidiabetic, antioxidant, and antibacterial activities of Acacia catechu (Lf) willd. Biomed Research International. 2021; 2021:758871. https://doi.org/10.1155/2021/7588711
75. Adhikari B, Aryal B, Bhattarai BR. A Comprehensive Review on the Chemical Composition and Pharmacological Activities of Acacia catechu (Lf) Willd. Journal Of Chemistry. 2021;2021:1-1. https://doi.org/10.1155/2021/2575598
76. Yadav V, Krishnan A, Vohora D. A systematic review on Piper longum L.: Bridging traditional knowledge and pharmacological evidence for future translational research. Journal Of Ethnopharmacology. 2020;247:112255. https://doi.org/10.1016/j.jep.2019.112255
77. Nabi SA, Kasetti RB, Sirasanagandla S, et al. Antidiabetic and antihyperlipidemic activity of Piper longum root aqueous extract in STZ induced diabetic rats. BMC Complementary And Alternative Medicine. 2013;13:1-9. https://doi.org/10.1186/1472-6882-13-37
78. Gou GH, Liu L, Abdubakiev S, et al. Anti‐Diabetic Effects and Molecular Mechanisms of Amide Alkaloids from Piper longum Based on Network Pharmacology Integrated with Cellular Assays. Chemistry & Biodiversity. 2023;20(1):e202200904. https://doi.org/10.1002/cbdv.202200904
79. Antora RA, Salleh RM. Antihyperglycemic effect of Ocimum plants: A short review. Asian Pacific Journal Of Tropical Biomedicine. 2017 Aug 1;7(8):755-9. https://doi.org/10.1016/j.apjtb.2017.07.010
80. Dai Y, Chen SR, Chai L, et al. Overview of pharmacological activities of Andrographis paniculata and its major compound andrographolide. Critical Reviews In Food Science And Nutrition. 2019;59(sup1):S17-29. https://doi.org/10.1080/10408398.2018.1501657
81. Suemanotham N, Phochantachinda S, Chatchaisak D, et al. Antidiabetic effects of Andrographis paniculata supplementation on biochemical parameters, inflammatory responses, and oxidative stress in canine diabetes. Frontiers In Pharmacology. 2023; 14:1077228. https://doi.org/10.3389/fphar.2023.1077228
82. Danao K, Kale S, Rokde V, et al. In Silico Prediction of Antidiabetic Activity of Phytoconstituents of Pterocarpus Marsupium Targeting α-Amylase Enzyme. Biosciences Biotechnology Research Asia. 2023;20(1):147-62. doi: http://dx.doi.org/10.13005/bbra/3077
83. Mishra A, Srivastava R, Srivastava SP, et al. Antidiabetic activity of heart wood of Pterocarpus marsupium Roxb. and analysis of phytoconstituents. Indian J Exp Biol. 2013;51(5):363-374.
84. Sarup P, Bala S, Kamboj S. Pharmacology and phytochemistry of oleo-gum resin of Commiphora wightii (Guggulu). Scientifica. 2015;2015. https://doi.org/10.1155/2015/138039
85. Kunnumakkara AB, Banik K, Bordoloi D, et al. Googling the Guggul (Commiphora and Boswellia) for prevention of chronic diseases. Frontiers In Pharmacology. 2018;9:686. https://doi.org/10.3389/fphar.2018.00686
86. Bhardwaj M, Soni A, Mishra S, Tripathi S. Protective effect of Commiphora wightii in metabolic activity of streptozotocin (STZ) induced diabetes in rats. J Diabetes Endocrinol. 2014;5(3):19-28. https://doi.org/10.5897/JDE2014.0076
87. Wikipedia. Boerhavia diffusa. Available at: https://en.wikipedia.org/w/index.php?title=Boerhavia_diffusa&oldid=1132791115
88. Kaur H. Boerhaavia diffusa: bioactive compounds and pharmacological activities. Biomedical And Pharmacology Journal. 2019;12(4):1675-82. https://dx.doi.org/10.13005/bpj/1797
89. Govindasamy C, Al-Numair KS, Alsaif MA, Viswanathan KP. Influence of 3-hydroxymethyl xylitol, a novel antidiabetic compound isolated from Casearia esculenta (Roxb.) root, on glycoprotein components in streptozotocin-diabetic rats. Journal Of Asian Natural Products Research. 2011;13(8):700-6. https://doi.org/10.1080/10286020.2011.585157
90. Deokate UA, Khadabadi SS. Phytopharmacological aspects of Salacia chinensis. Journal Of Pharmacognosy And Phytotherapy. 2012;4(1):1-5. doi: http://dx.doi.org/10.5897/JPP11.006
91. Chandramohan G, Al‐Numair KS, Sridevi M, Pugalendi KV. Antihyperlipidemic activity of 3‐hydroxymethyl xylitol, a novel antidiabetic compound isolated from Casearia esculenta (Roxb.) root, in streptozotocin‐diabetic rats. Journal Of Biochemical And Molecular Toxicology. 2010;24(2):95-101. https://doi.org/10.1002/jbt.20317
92. Kshirsagar PR, Jagtap UB, Gaikwad NB, Bapat VA. Ethanopharmacology, phytochemistry and pharmacology of medicinally potent genus Swertia: An update. South African Journal Of Botany. 2019 Aug 1; 124:444-83. https://doi.org/10.1016/j.sajb.2019.05.030
93. Dhyani P, Giri L, Sharma E, Sati P. Swertia chirayita, an Endangered Anti-diabetic Plant: Trends in Biotechnological Interventions. Biotechnology Of Anti-Diabetic Medicinal Plants. 2021:133-51. doi : https://doi.org/10.1007/978-981-16-3529-8_6
94. Kaur P, Pandey DK, Dey A, et al. Swertia spp.: A potential source of high-value bioactive components, pharmacology, and analytical techniques. Bioactive Natural Products In Drug Discovery. 2020:165-213. https://doi.org/10.1007/978-981-15-1394-7_4
95. Sharma R, Amin H, Prajapati PK. Antidiabetic claims of Tinospora cordifolia (Willd.) Miers: critical appraisal and role in therapy. Asian Pacific Journal Of Tropical Biomedicine. 2015;5(1):68-78. https://doi.org/10.1016/S2221-1691(15)30173-8
96. Hekmatshoar Y, Özkan T, Saadat YR. Evidence for Health-Promoting Properties of Lepidium sativum L.: An Updated Comprehensive Review. Turkish Journal Of Pharmaceutical Sciences. 2022;19(6):714. https://doi.org/10.4274/tjps.galenos.2021.07504
97. Alqahtani FY, Aleanizy FS, Mahmoud AZ, et al. Chemical composition and antimicrobial, antioxidant, and anti-inflammatory activities of Lepidium sativum seed oil. Saudi Journal Of Biological Sciences. 2019;26(5):1089-92. https://doi.org/10.1016/j.sjbs.2018.05.007
98. Sharma P, Joshi T, Joshi T, et al. In silico screening of potential antidiabetic phytochemicals from Phyllanthus emblica against therapeutic targets of type 2 diabetes. Journal Of Ethnopharmacology. 2020;248:112268. https://doi.org/10.1016/j.jep.2019.112268
99. Saini R, Sharma N, Oladeji OS, et al. Traditional uses, bioactive composition, pharmacology, and toxicology of Phyllanthus emblica fruits: A comprehensive review. Journal Of Ethnopharmacology. 2022;282:114570. https://doi.org/10.1016/j.jep.2021.114570
100. Mohi-ud-din R, Mir RH, Wani TU, et al. Phytochemical and Pharmacological Properties of Picrorhiza Kurroa. InEdible Plants in Health and Diseases: Volume II: Phytochemical and Pharmacological Properties 2022 (pp. 399-423). Singapore: Springer Singapore. https://doi.org/10.1007/978-981-16-4959-2_13
101. Sharma N. Picrorhiza kurroa. InHimalayan Medicinal Plants 2021 Jan 1 (pp. 67-83). Academic Press. https://doi.org/10.1016/B978-0-12-823151-7.00011-8
102. Mwangi RW, Macharia JM, Wagara IN, Bence RL. The medicinal properties of Cassia fistula L: A review. Biomedicine & Pharmacotherapy. 2021;144:112240. https://doi.org/10.1016/j.biopha.2021.112240
103. Salehi B, Ata A, V. Anil Kumar N, et al. Antidiabetic potential of medicinal plants and their active components. Biomolecules. 2019;9(10):551. https://doi.org/10.3390/biom9100551
104. Indu S, Vijayalakshmi P, Selvaraj J, Rajalakshmi M. Novel triterpenoids from Cassia fistula stem bark depreciates STZ-induced detrimental changes in IRS-1/Akt-mediated insulin signaling mechanisms in type-1 diabetic rats. Molecules. 2021;26(22):6812. https://doi.org/10.3390/molecules26226812
105. Krolikiewicz-Renimel I, Michel T, Destandau E, et al. Protective effect of a Butea monosperma (Lam.) Taub. flowers extract against skin inflammation: antioxidant, anti-inflammatory and matrix metalloproteinases inhibitory activities. Journal Of Ethnopharmacology. 2013;148(2):537-43. https://doi.org/10.1016/j.jep.2013.05.001
106. Somani R, Kasture S, Singhai AK. Antidiabetic potential of Butea monosperma in rats. Fitoterapia. 2006;77(2):86-90. https://doi.org/10.1016/j.fitote.2005.11.003
107. Chhatre S, Nesari T, Somani G, et al. Phytopharmacological overview of Tribulus terrestris. Pharmacognosy Reviews. 2014;8(15):45. https://doi.org/10.4103/0973-7847.125530
108. Khalid A, Nadeem T, Khan MA, et al. In vitro evaluation of immunomodulatory, anti-diabetic, and anti-cancer molecular mechanisms of Tribulus terrestris extracts. Scientific Reports. 2022;12(1):22478. https://doi.org/10.1038/s41598-022-26742-6
109. Sani A, Tajik A, Seiiedi SS, et al. A review of the anti-diabetic potential of saffron. Nutrition And Metabolic Insights. 2022;15:11786388221095223. https://doi.org/10.1177/11786388221095223
110. Yaribeygi H, Zare V, Butler AE, et al. Antidiabetic potential of saffron and its active constituents. Journal Of Cellular Physiology. 2019;234(6):8610-7. https://doi.org/10.1002/jcp.27843
111. Sattar NA, Hussain F, Iqbal T, Sheikh MA. Determination of in vitro antidiabetic effects of Zingiber officinale Roscoe. Brazilian Journal Of Pharmaceutical Sciences. 2012;48:601-7. https://doi.org/10.1590/S1984-82502012000400003
112. Otunola GA, Afolayan AJ. A review of the antidiabetic activities of ginger. Ginger cultivation and its antimicrobial and pharmacological potentials. 2019. https://doi.org/10.5772/intechopen.88899
113. Li Y, Tran VH, Duke CC, Roufogalis BD. Preventive and protective properties of Zingiber officinale (ginger) in diabetes mellitus, diabetic complications, and associated lipid and other metabolic disorders: a brief review. Evidence-Based Complementary And Alternative Medicine. 2012;2012. https://doi.org/10.1155/2012/516870
114. Durg S, Bavage S, Shivaram SB. Withania somnifera (Indian ginseng) in diabetes mellitus: a systematic review and meta‐analysis of scientific evidence from experimental research to clinical application. Phytotherapy Research. 2020;34(5):1041-59. https://doi.org/10.1002/ptr.6589
115. Gorelick J, Rosenberg R, Smotrich A, et al. Hypoglycemic activity of withanolides and elicitated Withania somnifera. Phytochemistry. 2015; 116:283-9. https://doi.org/10.1016/j.phytochem.2015.02.029
116. Tyagi R, Gupta V, Kumar R, Wander GS. Traditional Indian practices: Time to revisit and re-adopt for a healthier lifestyle, J Anaesthesiol Clin Pharmacol. 2020;36(Suppl 1):S166-S171. https://doi.org/10.4103/joacp.JOACP_299_20
117. Gherasim A, Arhire LI, Niță O, et al. The relationship between lifestyle components and dietary patterns. Proceedings of the Nutrition Society. 2020;79(3):311-323. https://doi.org/10.1017/S0029665120006898
118. Barani M, Sangiovanni E, Angarano M, et al. Phytosomes as innovative delivery systems for phytochemicals: A comprehensive review of literature. International journal of nanomedicine 2021;16:6983-7022. doi: https://doi.org/10.2147/IJN.S318416
119. Hu Y, Lin Q, Zhao H, et al. Bioaccessibility and bioavailability of phytochemicals: Influencing factors, improvements, and evaluations. Food Hydrocolloids. 2022;135(1):108165. https://doi.org/10.1016/j.foodhyd.2022.108165
120. Gunasekaran T, Haile T, Nigusse T, Dhanaraju MD. Nanotechnology: an effective tool for enhancing bioavailability and bioactivity of phytomedicine. Asian Pacific journal of tropical biomedicine. 2014;4(Suppl 1):S1-S7. https://doi.org/10.12980/APJTB.4.2014C980
121. Allegra S, De Francia S, Turco F, et al. Phytotherapy and Drugs: Can Their Interactions Increase Side Effects in Cancer Patients? Journal of Xenobiotics. 2023;13(1):75-89. https://doi.org/10.3390/jox13010007
122. Jităreanu, A., Trifan, A., Vieriu, M., et al. Current trends in toxicity assessment of herbal medicines: A narrative review. Processes. 2023;11(1):83. https://doi.org/10.3390/pr11010083
About the Authors
S. KumarIndia
Sachin Kumar - Assistant Professor.
Dehradun, Uttarakhand
Competing Interests:
No competing Interests.
A. Kumar
India
Ashok Kumar - Professor.
Raipur, Chhattisgarh
Competing Interests:
No competing interests.
J. Tantray
India
Junaid Tantray - Assistant Professor.
Jaipur, Rajasthan
Competing Interests:
нет
A. Shukla
India
Aman Shukla - PhD Scholar.
Dehradun, Uttarakhand,
Competing Interests:
No competing interests.
Supplementary files
|
|
1. Figure 1. Basic types and Causes of Diabetes mellitus. | |
| Subject | ||
| Type | Исследовательские инструменты | |
View
(318KB)
|
Indexing metadata ▾ | |
|
|
2. Figure 2. Pathophysiology of Diabetes Mellitus | |
| Subject | ||
| Type | Исследовательские инструменты | |
View
(267KB)
|
Indexing metadata ▾ | |
Review
For citations:
Kumar S., Kumar A., Tantray J., Shukla A. Ethnopharmacological Insights into Diabetes Management: Exploring Medicinal Flora of Shivalik range of Himalaya in Uttarakhand. Diabetes mellitus. 2024;27(5):498-509. https://doi.org/10.14341/DM13080

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).















































