Scroll to:
Comparison of Self-Management between Glycemic Controlled and Uncontrolled Type -2 Diabetic Elderly in Thailand: A Qualitative Study
https://doi.org/10.14341/DM12417
Abstract
BACKGROUND: For the past few decades, there have not been many studies done regarding diabetic patients’ perspectives. Diabetes mellitus is serious long-term care required for older patients. The facilitators have an important role in supporting diabetes patients.
AIM: The study aimed to assess and compare patients’ and caregivers’ perception of diabetes self-monitoring (DSM) and affects the Diabetes Self-Management Instrument (DSMI) of type-2 diabetic patients in both glycemic controlled and uncontrolled patients.
MATERIALS AND METHODS: The descriptive cross-sectional qualitative method was used to gather data from 25 participants among type II diabetes patients. Patients were recruited from the outpatient diabetes clinics in southern Thailand. Data were collected using a semi-structured in-depth interview guide and the focus group discussion. A thematic analysis approach was used to process the data.
RESULTS: From this study, 60% of the participants were among the uncontrolled glycemic group while 40% were the controlled group. The controlled group was found to have better self-management in the five themes of a healthy diet, regular exercise, medication taking, and risk prevention than the uncontrolled group. T2DM elderly in a controlled group has self-awareness and diabetic management intention higher than the uncontrolled group. The patient’s attitudes revealed five themes described fours themes of diabetic self-management intentions as reasoning, deciding, acting, and evaluating to perform self-management of older T2DM patients.
CONCLUSION: The elderly T2DM in the glycemic control group had self-awareness and intended to manage their diabetes and received more family support than those who were unable to control their blood sugar levels. Perceptions of elderly diabetic patients, their caregivers, and health workers revealed a common concern for behavioral intentions: obtaining self-care support from healthcare professionals and their families were the most important aspect of glycemic control in the elderly.
Keywords
For citations:
Wongrith P., Thiraratanasunthon P., Kaewsawat S., Le C.N. Comparison of Self-Management between Glycemic Controlled and Uncontrolled Type -2 Diabetic Elderly in Thailand: A Qualitative Study. Diabetes mellitus. 2022;25(2):174-185. https://doi.org/10.14341/DM12417
BACKGROUND
The prevalence of diabetes in older adults is increasing worldwide. According to the literature, the number of diabetic patients is projected to dramatically increase to 693 million by the year 2045 [1][2]. At that time, the number of type-2 diabetes mellitus (T2DM) patients would encompass around 90-95% of the population worldwide (with 49.7% of undiagnosed diabetes patients). Many adults aged > 65 years with DM have other chronic diseases that make management of their care more complex [3]. In 2015 the study reported that the total health expenditures spent on diabetic patients was as high as 673 billion USD and it was projected to increase to 802 billion USD in 2040 [4]. Thus, health care providers (HCPs) and caregivers play an important role in supporting DM patients (especially those in the higher age groups) [5][6]. This is because elderly patients face more difficulties in maintaining glycemic control, thus increasing the health risks and complications including the contraction of macrovascular and microvascular diseases [7][8].
In 2019, the study reported that only one-third of Asian patients from the previous study had adequately controlled T2DM with glycemic hemoglobin (A1C) levels, which is less than the recommended level of 7% [7][9]. Bureau of non-communicable disease, Ministry of Public Health (Thailand) reported the prevalence of diabetes per 100,000 population at 3,892 in 2016, 3,854 in 2017, and 4,059 in 2018. The proportions for patients who controlled (CP) over patients who unable to control their blood glycemic target (UP) were small rate as follows: 16/84 in 2014, 25/75 in 2015, 38/62 in 2016, 43/57 in 2017, and 44/56 in 2018, respectively. This, evidently, did not reach the goal of Thai IDF, which requires the proportion of CP to be more than 40% [4][10][11]. According to Thai diabetes guidelines (2017), older patients with comorbidities need to achieve certain goals to lead a quality life: maintaining Systolic Blood Pressure-SBP/ Diastolic Blood Pressure- DBP) < 140/90 mmHg, A1C 7.0-7.5% [10]. This is in line with the guidelines set by ADA and IDF, which also emphasized the importance of self-management skills as one that greatly influences the quality of diabetic patients’ daily lives and raises the quality of life [12].
The grounded conceptualization applied the Theory of Planned Behavior (TPB by Ajzen, 1991: Fig. 1) in this study consists of; 1) the attitude or perception of diabetic patients, 2) facilitators or subjective norms, and 3) diabetic self-management intention (DSMI) that three features effecting to diabetes self-management behaviors (DSM) [13]. Previous reports described that the self-management challenges faced by diabetic patients were low health literacy, difficulties in changing habits, and perceived barriers in lack of support [14-16]. From previous studies, facilitators such as family members were shown to be significant supporting factors in diabetic self-care management [15-17]. Knowledge and understanding of diabetes self-management (DSM) are also necessary to ensure ideal glycemic control. The factors such as no adherence to medical advice, difficulty in changing old habits, and the lack of the motivation to exercise were also presented as barriers to DSM. The researcher chose the rural area located in the southern region of Thailand as the location for this study because the rural area selected has a small rate of blood glucose control patients, limited availability of data regarding the practice of self-management, and limited previous studies about patient’s and health provider’s perspectives on the subject of DSM.
RESEARCH AIM
The study aimed to assess and compare the patients’ and caregivers’ perception of DSM and affects the DSMI of type-2 diabetic patients in both glycemic controlled and uncontrolled patients.
MATERIALS AND METHODS
Study Design
Mixed method study designs were chosen for this study because they provide are in-depth insights into specific contexts and social situations. First, a cross-sectional –descriptive focused on the participants’ socio-demographic data, and their medical records including BMI, blood pressure (BP), blood chemistry (FPG, A1C), and comorbidity (HT, CVD, DLP, and others). IDF (2017) guideline presented the criteria of the target glycemic control of elderly people (age> 65 years) should consider the patient’s overall health to set treatment goals. Second, a qualitative study based on Ajzen’s TPB, compares the theme as the conceptual framework for this study can be seen in figure 1 (Fig. 1). T2DM patients who have controlled and unable to control their blood glucose were recruited to participate in the study, which was the second phase of the previous study [14]. So the twenty-five patients were informed and recruited into the process of the semi-structured IDIs. The facilitators including 25 caregivers and three health providers were also invited to participate in the FGDs in the next process to explore and compare the diabetic self-management experience.
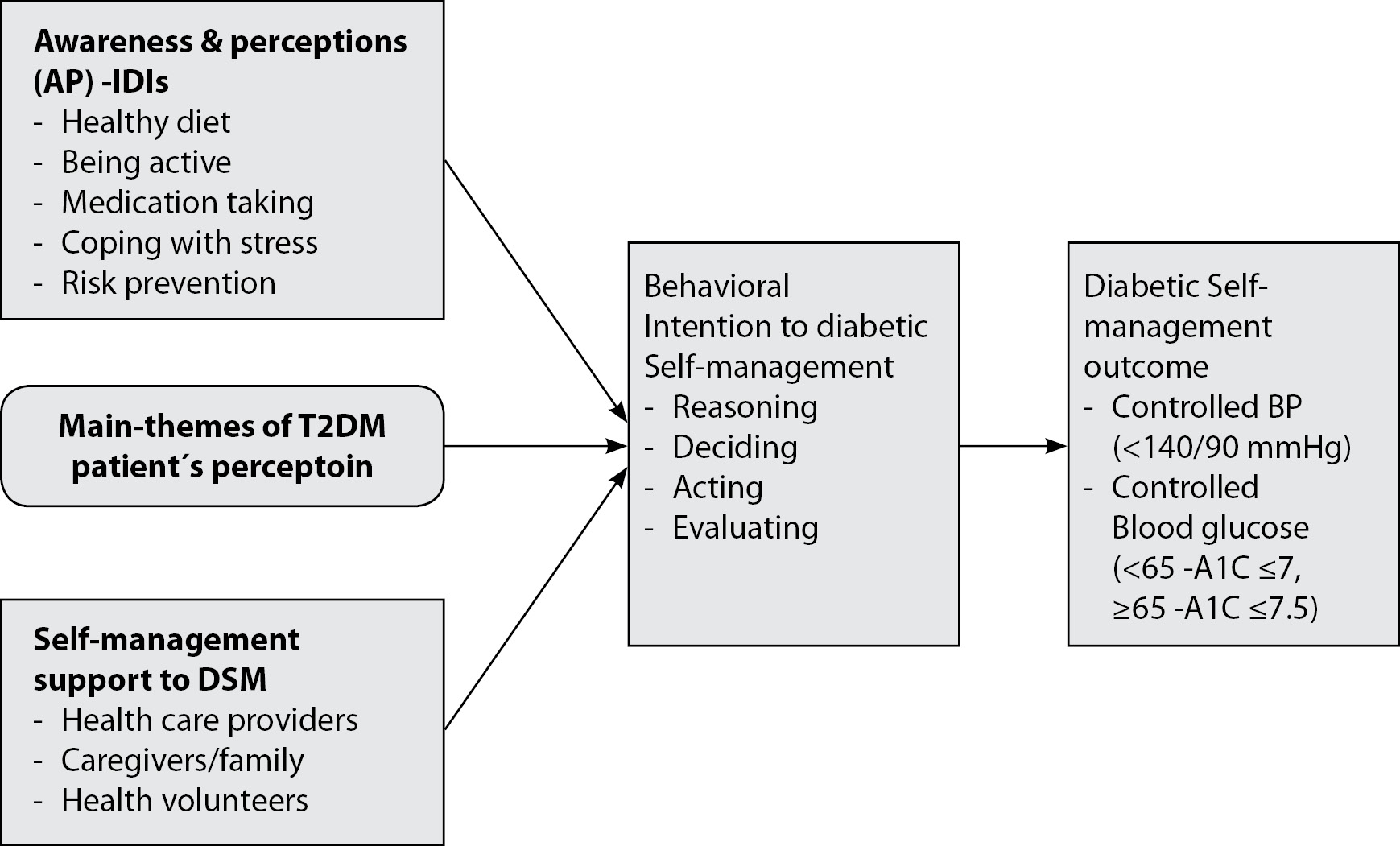
Fig. 1. Conceptual Framework.
Applied the Theory of Planned Behavior (TPB: Ajzen, 1991)
Place, context, and period of the research
Place of the research. This study was performed at the DM clinic Pak-Phanang Community Health Center in Nakhon Si Thammarat province, Southern Thailand. In the context and culture in the Southern region, people have traditional ways to follow their family lifestyle, and almost all extended families have their meals together with the same menu at home. On special occasions, whether an auspicious or sad event, people often gather together to cook and to eat multiply varieties of food. Accordingly, this situation also becomes difficult for diet control among diabetic people. Moreover, the young always make many kinds of food in any season to play how to respect to the older. Southern Thai style makes patients unable to control sweet foods and fatty foods, which may affect their self-management and cause multiple complications among T2DM patients.
Period of the research. This study was conducted in a 13-months duration, from May 2017 to December 2018. The data were collected in September 2017 and analyzed in December 2018.
Populations understudy
The study population was comprised of 212 T2DM patients previously diagnosed with T2DM who attended the Pak-Phanang Community Health Center.
Method of sampling from the studied population
As the aim of this study was to describe patients’ self-management practices, newly diagnosed patients were not included in this study.
Inclusion criteria: The criteria for being selected for the study is as follows: 1) both male and female T2DM, aged between 60-80 years old with no mental condition problem. 2) The participants were diagnosed with T2DM attendance at the DM-clinic at least 1 year, 3) Being treated with anti-diabetic medication for at least 6 months with laboratory data confirming their current health states, 4) They had comorbidities as hypertension, 5) They joined voluntarily in the study and, were able to talk and discuss through during the in-depth interview (IDIs) and focus group discussion (FGDs), and 6) Patients’ have caregivers who supporting as the informants to joined FGDs.
Exclusion criteria: 1) participants has had not finished the processes of IDIs and FGDs, and 2) the participants withdrew from the study in any reason. 25 final patients’ participants were selected to be informants through two steps of IDIs and FGDs. 25 caregivers were also asked for their consent to join the FGDs. Therefore, there were 50 final participants who informants participated in this qualitative study. A flowchart representation of patient selection of the study shown in figure 2 (Fig. 2).
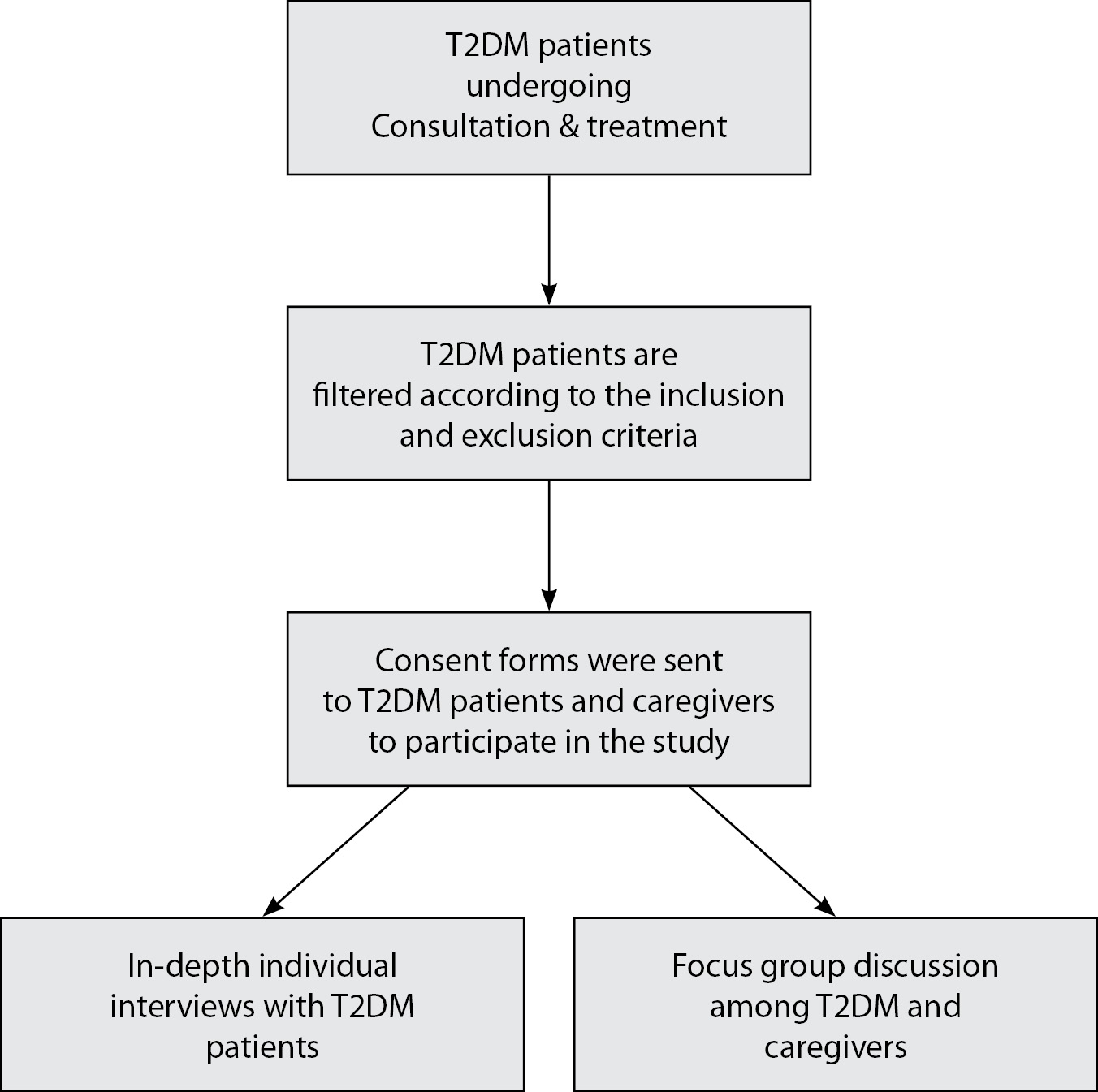
Fig. 2. Flowchart of sample selection number of samples enrolled in each group.
Data Analysis
The data gathered were then analyzed using the descriptive analysis method and thematic analysis method. Data from the elderly patient’s perceptions of T2DM self-management were collected and explored extensively. The descriptive Analysis method was chosen to present detailed information of the participants whereas the Thematic Analysis method was used to analyze and present participants’ perceptions according to specified themes.
Statistical analysis
The descriptive statistical analysis was examined, the percentages and averages were carried out. Microsoft Excel (2010) was used to determine five features of diabetic self-care management and the treatment outcome. The content analysis process and quality of the statistical analysis as follows;
1. The IDIs and FGDs were audiotaped recordings and transcribed verbatim, the reflection of facilitators and health providers was added, check the saturation of the data, and confirm the facts by informants.
2. Meaningful parts were identified by three technicians (Nurse practitioner (NP); healthy diet, being active, Pharmacist (PC); drug compliance, family medical doctor (FMD); coping with stress and risk prevention).
3. Formed meaning units in the text were shortened and coded into the aspects of the conceptual under the contextual causal conditions. Subthemes were developed according to the correlations between meaning units.
4. Themes with similar concepts were grouped to form main themes.
5. The final application was discussed by the research team and in additional interpretation by triangular checking the validity and reliability to decrease misrepresentation and misinterpretation, we used different ways to increase the validity of findings.
Ethical review
The participants understood the purpose of the study and signed the informed consent form to allow audio recording during the process of IDIs and FGDs.
1.The written consent was obtained from the participants after they have been verbally agreed, capacity for self-direction, withdrawal at any time.
2.The full research project entitled “The Experience of self-care to control blood sugar levels in elderly with diabetes at Muang Pak - Phanang Community Health Center” with the report number 016/2560 on 15 January 2017.
3.Data was collected after the study protocol was approved by the ethics committee, Nakhon Si Thammarat, Provincial Health Office.
RESULTS
- The descriptive findings
1.1 Participant’s clinical health information
The total number of participants of this study consists of 25 T2DM patients, mean aged 68.28±5.48 years, DM duration at 7.36±4.31 years, with slightly overweight with BMI of 24.49±2.64 and low monthly income 9,000±5,829THB (287USD). 14 out of 25 of the participants belonged to the UP group while 11 belonged to the CP group. More than half of both CP-UP groups were had ages over 65 years. More detail was presented in Table 1.
Blood pressure monitoring: Both groups able to control blood pressure under criteria that SBP <140 mmHg, DBP <90 mmHg during one year of monitoring. The average SBP showed the majority in well-controlled (138±7.53 mmHg), while DBP showed completely controlled in both groups (77.22±5.08 mmhg). Most of all in CP group can control target blood pressure, while about half in the UP group can control blood pressure (Table 2).
FBG- HbA1C monitoring: The patient’s FBG was presented to all participants to check the FBG trend. The means of fasting blood glucose monitoring and five times every 3 months during the year 2017 were demonstrated in the uncontrolled group. The participants three of fourth uncontrolled the glycemic target (76.0%). The maximum-minimum of FBG at 468, 70 mg/dl, respectively (Table 3). The trend of average FBG in all participants is slightly uncontrolled with an average FBG 146±19.92 mg/dl (Fig. 3.1). The A1C had been monitoring three times yearly from September 2017 to September 2019. The glycemic outcome between controlled and uncontrolled showed similarly. On average, more than half of the participants were unable to achieve the glycemic target goal (56%) (Table 3). The trend of average A1C (7.2±1.01%) was controlled under elderly DM criteria (<7.5%) (Fig. 3.).
Table 1. Demographic and clinical characteristics of participants (n = 25)
Personal factors | Character | Controlled (n=11) | Uncontrolled (n=14) | Min | Max | Mean | SD | ||
Cases | % | Cases | % | ||||||
Age (years) | <65 | 5 | 45.5 | 4 | 28.6 | 60.0 | 79.0 | 68.28 | 5.48 |
≥65 | 6 | 54.5 | 10 | 71.4 | |||||
BMI (kg/ m2) | ≤24.9 | 6 | 54.5 | 8 | 57.1 | 20.0 | 29.8 | 24.49 | 2.64 |
>25.0 | 5 | 45.5 | 6 | 42.9 | |||||
Income (Baht) | ≤ 5000 | 2 | 18.2 | 6 | 42.9 | 2,000 | 20,000 | 9,000 | 5,829.16 |
5001-10,000 | 4 | 36.4 | 4 | 28.6 | |||||
>10,001 | 5 | 45.5 | 4 | 28.6 | |||||
Duration (years) | ≤5 | 5 | 45.5 | 4 | 28.6 | 2.0 | 18.0 | 7.36 | 4.31 |
>5 | 6 | 54.5 | 10 | 71.4 | |||||
sex | Male | 4 | 36.4 | 2 | 14.3 | ||||
Female | 7 | 63.6 | 12 | 85.7 | |||||
status | Single | 2 | 18.2 | 6 | 42.9 | ||||
Married | 9 | 81.8 | 8 | 57.1 | |||||
Occupation | Not work | 2 | 18.2 | 7 | 50.0 | ||||
Merchant | 7 | 63.6 | 5 | 35.7 | |||||
Employment | 2 | 18.2 | 2 | 14.3 | |||||
Caregiver | Spouse | 6 | 54.5 | 9 | 64.3 | ||||
Son/daughter | 3 | 27.3 | 4 | 28.6 | |||||
VHVs | 1 | 9.1 | 2 | 14.3 | |||||
Comorbidity | HT | 11 | 100.0 | 14 | 100.0 | ||||
DLP | 11 | 100.0 | 14 | 100.0 | |||||
DN | 10 | 90.9 | 10 | 71.4 | |||||
CVD (Heart, IHD) | 1 | 9.1 | 4 | 28.6 | |||||
Complication | No | 7 | 63.6 | 7 | 50.0 | ||||
Yes-hypoglycemia | 3 | 27.3 | 4 | 28.6 | |||||
Yes-Hyperglycemia | 1 | 9.1 | 4 | 28.6 | |||||
Note: BMI –Body Mass index; VHVs-village health volunteers; HT-Hypertension; DLP-Dyslipidemia; DN-Diabetic nephropathy; CVD- cerebrovascular disease
Table 2. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) (n=25)
Blood pressure | Controlled n=11 | Uncontrolled | Participant’s Blood pressure n=25 | |||||
yes | No | yes | No | Min | Max | Mean | SD | |
B1-Systole | 10 | 1 | 7 | 7 | 105.0 | 158.0 | 134.24 | 13.98 |
-Diastole | 9 | 2 | 6 | 8 | 64.0 | 95.0 | 78.04 | 8.18 |
B2-systole | 10 | 1 | 6 | 8 | 112.0 | 154.0 | 136.24 | 10.91 |
-Diastole | 10 | 1 | 8 | 6 | 60.0 | 87.0 | 74.32 | 7.95 |
B3-Systole | 9 | 2 | 9 | 5 | 123.0 | 166.0 | 137.92 | 10.61 |
-Diastole | 10 | 1 | 6 | 8 | 65.0 | 98.0 | 78.36 | 8.47 |
B4-Systole | 8 | 3 | 6 | 8 | 114.0 | 167.0 | 141.40 | 14.20 |
-Diastole | 9 | 2 | 7 | 7 | 65.0 | 94.0 | 77.24 | 8.17 |
B5-Systole | 7 | 4 | 6 | 8 | 114.0 | 159.0 | 140.20 | 11.37 |
-Diastole | 10 | 1 | 9 | 5 | 68.0 | 95.0 | 78.16 | 6.80 |
Average -SBP | 8.8 | 2.2 | 6.8 | 7.2 | 119.0 | 153.0 | 138.0 | 7.53 |
Average -DBP | 9.6 | 1.4 | 7.2 | 6.8 | 67.0 | 88.0 | 77.22 | 5.08 |
Note: Controlled SBP <140mmHg, DBP <90mmHg; uncontrolled SBP ≥140mmHg, DBP ≥90mmHg (Criteria of older at 65 years by IDF, 2017)
B1-B5 -Blood pressure were coded from Health record every 2 months, May 2017, July 2017, September 2017, November 2017, January 2018
Table 3. Fasting blood glucose (FBG) and glycosylated hemoglobin (A1C) (n=25)
Glycemic level | Controlled | Uncontrolled | Min | Max | Mean | SD | ||
n | % | n | % | |||||
FBG1 | 5 | 20.0 | 20 | 80.0 | 70 | 208 | 135 | 27.19 |
FBG2 | 6 | 24.0 | 19 | 76.0 | 93 | 247 | 156 | 45.34 |
FBG3 | 5 | 20.0 | 20 | 80.0 | 92 | 468 | 159 | 70.26 |
FBG4 | 10 | 40.0 | 15 | 60.0 | 91 | 228 | 143 | 33.81 |
FBG5 | 12 | 48.0 | 13 | 52.0 | 93 | 248 | 137 | 33.35 |
Average FBG | 6 | 24.0 | 19 | 76.0 | 99 | 197 | 146 | 19.92 |
A1C2017 | 15 | 60.0 | 10 | 40.0 | 5.4 | 9.6 | 7.3 | 1.04 |
A1C2018 | 12 | 48.0 | 13 | 52.0 | 5.7 | 10.4 | 7.3 | 1.12 |
A1C2019 | 13 | 52.0 | 12 | 48.0 | 5.7 | 10.0 | 7.4 | 1.03 |
AverageA1C | 11 | 44.0 | 14 | 56.0 | 4.80 | 9.30 | 7.2 | 1.01 |
Note: Controlled FBG ≤150 mg/dl, A1C 7-7.5%, uncontrolled FBG>150 mg/dl, A1C >7.5%
FBG 1-5- were coded from FBG record every 2 month (May 2017, July 2017, September 2017, November 2017, and January 2018); A1C were coded from (Hemoglobin A1C) yearly monitoring by 2017-2019
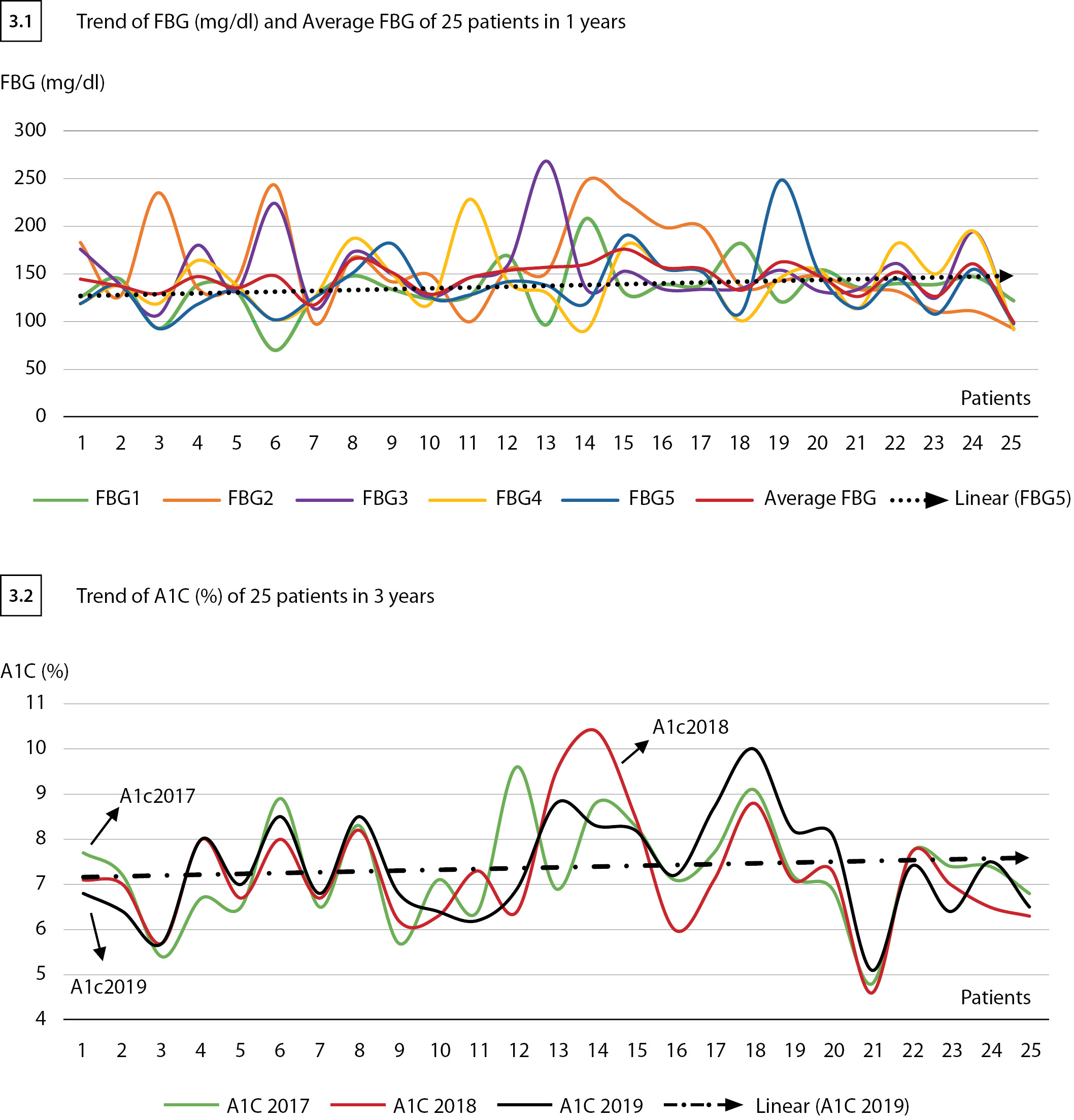
Fig. 3. Trend of FBG and A1C (%) of 25 patients.
1.2 Attitudes towards self-care management: An in-depth interview
Patients’ perceptions were reported in five aspects are healthy diet that most of CP agreed with healthy food consumed whereas UP had agreed in low fat only. In being active, more than half of CP agreed in both regular exercise and acts in physical activities, but 12 cases disagreed in being active. In aspects of coping with stress, all of CP agreed with effective stress management, while 9 cases of UP unable to cope with stress. In risk prevention, both CP-UP agreed with no smoking and no drinking but 10 cases UP groups disagree in continuity blood pressure control. In medication adherence, most of all patients in the controlled group agree with drug compliance and follow-up doctor plan treatment, whereas 10 cases in the UP group had loss follow up (Table 4). In drug compliance, of 15 cases participants in both groups used two or more anti-diabetic drugs as biguanide (Metformin) and sulfonylureas (Glipizide) because both drugs had no problem with chronic kidney disease 3rd stage. Most of patients used anti-hypertensive drug as, Thiazide, Enalapril, and Amlodipine. The other drugs that most of the patients were received such as Statin for decrease LDL (not exceed 100 mg/dl) and serum cholesterol (not exceed 200 mg/dl), all of the participants had ASA grain 81 for cerebrovascular prophylaxis.
Table 4. Patient’s attitudes from In-depth interview (n=25)
Themes | Sub-themes | Agree | Disagree | Controlled Group | Uncontrolled Group [n=14] | ||||
Desirable behavior | n | % | n | % | Agree | Disagree | Agree | Disagree | |
Healthy diet | Low Carb | 18 | 72.0 | 7 | 28.0 | 9 | 2 | 9 | 5 |
Low Sweet | 19 | 76.0 | 6 | 24.0 | 11 | 0 | 8 | 6 | |
Low Fat | 10 | 40.0 | 15 | 60.0 | 6 | 5 | 4 | 10 | |
More Vegetable | 18 | 72.0 | 7 | 28.0 | 8 | 3 | 10 | 4 | |
Being active | Regular Exercise | 8 | 32.0 | 17 | 68.0 | 6 | 5 | 2 | 12 |
Physical Activity | 16 | 64.0 | 9 | 36.0 | 7 | 4 | 9 | 5 | |
Coping with stress | Stress management | 16 | 64.0 | 9 | 36.0 | 11 | 0 | 5 | 9 |
Preventive risk | No smoking | 19 | 76.0 | 6 | 24.0 | 9 | 2 | 10 | 4 |
No drinking | 18 | 72.0 | 7 | 28.0 | 8 | 3 | 10 | 4 | |
BP controlled | 11 | 44.0 | 14 | 56.0 | 7 | 4 | 4 | 10 | |
Medication taking | drug compliance | 20 | 80.0 | 5 | 20.0 | 10 | 1 | 10 | 4 |
Follow up | 11 | 44.0 | 14 | 56.0 | 10 | 1 | 4 | 10 | |
Note: Sub-themes were coded exploratory from semi- structured in-depth interview form
- The qualitative themes findings; their findings were very different, so these themes were gained; Patients’ perception affecting the Self-management intention-DSMI categorized by the HbA1cas controlled patients (CP) and uncontrolled patients (UP).
2.1 Perception of T2DM patients (AP) and Self-management Intention-DSMI
1) Controlled patients (CP)
AP — Dietaries habits was said “Patients know and aware of good diet then they intend to practice.”
AP — Active lifestyles was said “Just movement, do not stop exercising because we grow old, we grow old because we stop exercising.”
AP — Stress management effectiveness was said “Emotional stress and anxiety causing high blood sugar”
AP — risk Prevention was said “Preventive risk as no smoking and no drinking is the best way to live with diabetes.”
AP — Drug compliance Patients was said “Taking medication, understanding and follow doctors’ prescribed.” Patients was said “If doctors have continued support, they will be easier to long-term practice”. HCPs was said “If they adherence and continue practice follow doctors’ advice, they will be controlled blood glucose.”
2) Uncontrolled patients (UP)
AP — Dietaries habits: “I know what I should eat but don’t know the exact amount to eat.”, “Loose of self-control for an events meeting and a lot of friends urge.”
AP — Active lifestyles: “Trying to exercise but not seeing any progress and so many barriers”,
“Unable to cope with the stress of health as being and showing signs and serious symptoms”.
AP — Stress management effectiveness Patients: “Family support can reduce emotional stress and anxiety”
AP — risk Prevention: “No concern in risk prevention out of control blood sugar.”
HCPs: “Expecting being supported from family and health provider”
AP — Drug compliance Patients: “Follow prescription make better blood glucose”
Patient’s perception: The in-depth interviews were transcribed and coded using a content analysis approach to identify themes in the self-care of patients. The following figure compared the themes of controlled and uncontrolled groups. “No concern in risk prevention, out of control blood sugar.” and “Preventive risk as no smoking no drinking is the best way to live with diabetes.” were similarly expressed by both groups. The results showed Most of the CP group had perceived the beneficial good diet, regular exercise, drug adherence, and risk prevention than the UP group (Fig. 4.).
2.2 Caregiver’s and HCPs views of Self-management support:
Apply for diabetic self-management support by coding to describe barriers or situations patient faces that make it difficult to initiate and sustain the self-management of behaviors that improve type 2 diabetes condition. Social support refers to reference groups of people who support the patients do self-activities. Focus group discussion among patients, caregivers, and health providers was transcribed and themes were approached. The themes were presented in the same way that the HCP’s view was presented to the patients in the controlled group as “If they adherence and continue practice follow doctors’ advice, they will be controlled blood glucose”. On contrary, caregivers presented that most of the patients who unable to control complained they have not proper support from the health providers as “Expecting being supported by family and health provider”. In the same direction, the patients in the uncontrolled group said “Family support can reduce emotional stress and anxiety” (Fig. 4.).
2.3 Diabetic Self-Management Intention of patients (DSMI)
The findings showed both groups present the barriers in self-management but the controlled group had reasonable deciding and do action, while the uncontrolled present they were unable to practice and would like to stop all doctor prescriptions (Fig. 4.).
Self-management Intention -DSMI (CP)
Deciding: “Difficulties managing stress but desires to reduce and control blood sugar.”
Acting: “Behaviors were do not continue due to lack of progress.”
Evaluation: “I am unable to do self-blood glucose monitoring.”
Self-management Intention- DSMI (UP)
Reasoning-deciding: “Patients stopped self-management due to lack of progress.”
Acting: “Perceived great barriers and unwillingness make loss of self-control.”
Evaluation: “Family is not help or support of the patient need to control diet.”
The controlled group presented “Reasoning” as “More reasons and perceived benefits in risk prevention.” whereas the uncontrolled group had different beliefs, and for example, “Difficulties managing stress.” The intention theme in the controlled group in “Deciding” showed, “Other family members supporting and helping patients to diet control.” compare with the uncontrolled group presented that “family is not concerned or supportive or helping patients to diet control.”
The theme in the controlled group in “Acting” that, “No progress, No good outcome, and the behaviors were not continued.”, but the uncontrolled group showed that “Low expectation of support from friends and peers and perceived barriers rather than as benefits.” Moreover, the intention in “Evaluating” was presented “alternative medicine and functional food were more available but limited by financial reasons.” Alternately, the uncontrolled group showed, “Cannot do self- blood glucose monitoring.” More stated in the same way with HCP, “Patients do not perceive diabetes as serious.” (Fig. 4.). Therefore, the patient’s intentions to perform diabetic management in the controlled group demonstrated stronger than the uncontrolled group.

Fig. 4. Themes in the Patients’ perception and Self-management intention-DSMI.
DISCUSSION
Sample representatively
The qualitative is conducted with a small number of recruit patients. The analyzing data was depended on the content analysis method. So the findings not enough to be representativeness of the target populations. However, these results can be made more understanding the perception and key of success way of older diabetic self-management to enhance better quality of life.
The discussions were divided the T2DM into two categories with controlled and uncontrolled their glycemic follow by the A1C criteria above mentions and compared themes as follows.
- The trend of high rate glycemic uncontrolled
The trend of one-year average FBG and 3 years A1C in both groups demonstrated prominent as uncontrolled (Figure 3). The patients complained long-term of DM duration of more than six years that they had no willingness to control and unstable glycemic level in the middle range is associated with higher risk [6][12]. This trending predicted many of these patients are at increased risk of chronic complications, functional decline, disability, and mortality [12]. So facilitators must take efforts to reduce complications through glycemic control.
- The attitudes toward behavior as following Healthy diet
There were responses about the barriers to control diet/calories. Most of the patients were low income and this affects their eating habits, they tend to put what is in season and inexpensive. The uncontrolled patients stated that the elderly do not know the exact amount of carbs, fat, and salt per meal or per day, which results in the inability to control the glycemic level. Furthermore, the elderly prefer seasonal sweet fruits and cheap, so it’s become part of daily consumption that affecting increasing blood glycemic. Those patients did not have an awareness and how to control diet. Similarly with the themes of the previous study that “Diet challenges during social occasions” and the theme was “Diet control is not restricting” and Our study showed that patients with type 2 diabetes had an overall inappropriate dietary attitude [3][7], but in contrast, the majority of patients were on a strict diet [9]. However, their cultural backgrounds, personal preferences, co-occurring conditions, and socioeconomic settings in which they live would also affect the glycemic targets [5][14]. The culture of the Thai southern region, discussed of “eating” and “food” is traditionally not just to meet one’s “physical need” but they preferred to enjoy all kinds of delicious food after working hard for their entire life with family. Therefore, the elderly need more individual education, guidance, and appropriate support in diabetic diet [3]. Patients generally lack proper information/knowledge regarding the dietaries habits and how they should be implemented.
Being active
The findings presented physical exercise recommendations were inadequately practiced by most of the participants, especially in the uncontrolled group. Patient’s attitudes which were expressed from a controlled participant contrasted with the uncontrolled expression in being active [3][7]. Further, almost 59% of patients reported frequent exercise, similarly with the controlled patients in this study that most of them preferred daily walking [6]. On the other hand, patients in the uncontrolled group had the misconception, no awareness, and poor health status that unable to work with regular exercise. Not only had that but also perceived many barriers such as disability, low economic, and low family support. Thus, patients with a physical disability required extensive care and effective strategies to control glucose metabolism higher than the controlled patients.
Coping with stress
The controlled theme expressed, stress and anxiety cause high blood sugar, but the uncontrolled presented that they were usably coping with the stress. The elderly have ways to relieve stress by doing hobbies, practicing religious activities, exercising, and talking to friends [7]. However, older with poor health, low income, and lack of support from family were unable to perform self-management. Perceived coping stress associated with anxiety and time since diagnosis [7]. These data could be useful to plan T2DM psychological intervention focused on psychological health concerns, leading to healthy self-management [12].
Medication adherence
The prescribed medications are a significant predictor of glycemic control of older T2DM patients. The controlled and uncontrolled also demonstrated, the understanding and follow doctor’s advice was consistent with taking medication as the best way to make blood sugar levels drop and believed that this would prevent complications [12][14]. Few uncontrolled patients had reported signs of hypoglycemia after taking sulfonylurea 1-2 times a month that consistent with the report that 25% of the hypoglycemia is reported, and change to a drug with a short half-life, such as glipizide, is recommended by IDF (2019). Which consistently with Sulfonylureas should be avoided in older adults due to the high risk of hypoglycemia [12]. Taking medication as prescribed with adjusting the diet by reducing the amount of food intake and choosing the type of food consume found improving or maintaining glycemic target. The loss follows up was reported in uncontrolled that consequence with doctors notes that most of the uncontrolled patient disappear three or four months and reappear with serious complication [7]. This was caused by participants’ lack of proper knowledge and perception on diabetes adherence to medications. Healthcare providers should explore to better understand patients’ perspectives on diabetes, and provide more effective health education interventions to enhance medication adherence.
Complication prevention
The attitudes are internal barriers and individual choices that need to change [13]. Support with the desired behaviors in people with diabetes that predict good outcomes [15]. Attitudes predicted behaviors, lead to good glycemic control and long-term improvement of quality of life. Healthy diet and exercise are important in complication prevention for older DM with more comorbidities [7]. In addition, no smoking or no drinking, and follow doctor’s comply were also needed [7]. Accordingly, the controlled group had better accomplish than the uncontrolled. To sum up, most participants in controlled groups agreed to the importance of self-management practices especially healthy eating, exercise, taking medications, and healthy coping with stress to control DM and prevent its complications.
- Themes comparing in the glycemic controlled patient and uncontrolled patients
Diabetic Self-management Intention
The main objective of this study is to explore the impacts that explain the behavioral intention of the T2DM elderly in four aspects including, reasoning, deciding, acting, and evaluating through the IDIs.
Reasoning: Although, the controlled groups presented their perceptions in the same way with the uncontrolled group about “risk Prevention” but they demonstrated the different reasoning to negative deciding to do exercise or diabetic diet control. However, they stated no smoking in both groups that influence perceptions about the susceptibility and cause complications from their reasoning [14]. The controlled group had better management in a healthy diet, regular exercise, medication taking, and risk prevention than the uncontrolled group. However, they still need support as reasoning as “If doctors have continued support, they will be easier to long-term practice”. Consequently, lower self-management was caused by unsure expected benefits and efficacy of treatment from they decided to not acting in the uncontrolled group [8][14].
Deciding: The patient in the controlled group had performed self –management decided to “Difficulties managing stress but desires to reduce and control blood sugar.” On the contrary, patients in uncontrolled stated that “Behaviors were do not continue due to lack of progress.” Facilitating conditions have a significantly positive relationship with the intention to adopt a diabetic management application. Thus, supporting my caregiver, nurses, physicians, and community health works as village health volunteers is key to success in elderly diabetic self-management.
Acting: Patients in the uncontrolled group stated that they were unable to resist fatigue as hypoglycemia, and they no antidiabetic adherence. Poor adherence to medication leads to increased morbidity and death and raises costs of expense. The attitudes were strong predictors and support the patient’s behavioral intentions. To predict adherence to the use of oral antidiabetic methods, and follow the clinician’s treatment plan [10][14]. The power of a small group sharing and discussion, time to share, clarify suggest and expand concepts were made patients learning to have desirable self-management. The recommendation for effective intervention for health providers should be multi-component and provide adequate contact time (>10 hours) with continuity through community-based [10][20]. There have been reports of studies in people with type 2 diabetes who have poor control over diabetes. Structural self-monitoring blood glucose (SMBG) is performed 7 times a day for 3 days in a row. Food intake is recorded [2]. Exercising every 3 months with a doctor’s visit can reduce A1C by 0.3%. The positive attitudes of providers, important subjective norms, and perceived behavioral control in barriers or benefits of diabetes patients had a positive effect on the intention of DSME [15]. Therefore, diabetic caregivers and care providers should focus on older patients and continuously support self-management [12]. The empowerment and support from health professionals, and family is also important for patients is recommended to enhance glycemic control.
Evaluating: Most of the patients in both groups have evaluated with the stated that “Behaviors were not continuing due to lack of progress.” Whereas, the HCP concerned that “Patients aren’t interested in risk prevention.” (HCP). WHO presented the caused factors were complex such as disease-related factors, therapy-related factors, and patient-related factors.
This is in line with the explaining of the theory of planned behavior that intention to do something is the significant factor in behavioral modification.
The Diabetic Self-management support (DSMS)
This study found similarly that significant facilitators in the elderly including family members, health volunteers (VHVs), and health care providers (HCPs) [12][16]. They gathering support information sharing, improving daily life, and intercommunicating patient’s needs through the cultural beliefs [17]. Family support is well known as Thai culture and is essential for Thai rural society [8]. The elderly were often visited by many relatives and friends in a traditional day with various foods that interrupted a healthy diet in both controlled and uncontrolled. However, they have a responsibility to receive the food given to them ever when they know it is unhealthy for diabetics [3][8]. Therefore, family caregiver and HCPs are the main support and important in overcoming negative behaviors and optimizing behaviors in diabetes control [9][14]. The uncontrolled patients discussed a lack of family support, while the controlled patients have competency in self-management [7]. The controlled patients revealing expectations, because of daily care in diabetes is handled by patients and/or families, especially for the elderly who are often dependent on others [17]. The consequence with family members is beneficial to improve adherence to the lifestyle, drug adherence, and avoid complications [7][18]. On the other hand, HCPs perceived that uncontrolled blood glucose of patients’ cause of they are non-drugs adherence and unfollow doctors’ advice [7]. Many studies found that T2DM adherence was influenced by positive feedback mechanisms occurring from internal or external motivational factors resulting from supportive interactions, social relationships, or the person’s ability to cope with situations [19]. So, Health providers and patients should develop mutually agreed-on goals that are reasonable and practical to implement and also address the lack of involvement or empowerment to help and motivate patient concern and action [3][19]. Therefore, Patients found it difficult to lifestyle modification otherwise, Healthcare providers recognized that patients needed support to change behavior, but have inadequate readiness to change [19][20]. So, supporting self-management strategies for successful aims were empowering, healthcare professionals re-evaluating the provision of short term self-management education and support in routine care especially in elderly T2DM patient who lack of glycemic control.
Comparison with other publications
This qualitative of the past study was similarly with Pamungkas RA, et al [14] that focus on Diabetes mellitus self-management (DMSM) and its purpose to maintain blood glucose levels.
Clinical significance of results
The strength of this qualitative study was the comparative experience of individual diabetic self-management through the in-depth interview and focus group discussion to understand patients’ views both controlled and uncontrolled group.
Limitations of the research
The primary limitation was the small sample size in this study, 25 patients’ and 25 caregivers, was difficult to identify significant relationships. Moreover, we recognize that other variables that possibly influence self-management adherence.
Directions for further research
The next study should focus on the self-management support intervention and patient-center scale-up about the diet health literacy, SMBG, and alternative exercise for older T2DM and caregivers.
CONCLUSION
This study demonstrated the effect of perceptions and behavioral intention on improving self-management in older patients with diabetes both in the controlled and uncontrolled glycemic group. Healthcare providers should mark and pay attention to facilitate the diabetic self-management program both at a community level or at Health Care Center.
OTHER INFORMATION
The source of financing. The source of financing. “This research was initiated through a support grant from Pak- Phanang Municipality Health Fund, NHSO, and partially supported by the Research Institute, Walailak University, and the EC for DACH excellence center.
Conflicts of interests. “The authors declare that there are no obvious or potential conflicts of interest associated with the publication of this article.”
Participation of authors. All author has participated to the research and preparation of the article in four criteria as followed:
1. P. Wongrith — Designed concept or study design and data analysis or interpreting results;
2. P. Wongrith, P. Thiraratasunthon, S. Kaewsawat, and C. Ngoc Le — Writing an article or making significant changes to the manuscript to increase the scientific value of the article;
3. All authors — Approval of the final version of the manuscript, and Consent to be responsible for all aspects of the work, which implies proper investigation and resolving of issues related to the accuracy or integrity of any part of the work.
Acknowledgments. Thanks to the public health teams at Pak-Phanang Community Health Centre who provided assistance and support in collecting medical records and tracking volunteers. This research was funded through a support grant from Pak Phanang Municipality Health Fund, NHSO, and partially supported by the new strategic research project, Walailak University, Thailand.
References
1. Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271-281. doi: https://doi.org/10.1016/j.diabres.2018.02.023
2. International Diabetes foundaration. Diabetes Atlas 9TH edition 2019. [Internet]. 2019. Available from: https://www.idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html
3. Rowe DS. Barriers to the Prevention and Treatment of Geriatric Diabetes. Fed Pract. 2015;32(S11):16S-20S.
4. Ogurtsova K, da Rocha Fernandes JD, Huang Y, et al. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40-50. doi: https://doi.org/10.1016/j.diabres.2017.03.024
5. Pamungkas R, Chamroonsawasdi K, Vatanasomboon P. A Systematic Review: Family Support Integrated with Diabetes Self-Management among Uncontrolled Type II Diabetes Mellitus Patients. Behav Sci (Basel). 2017;7(4):62. doi: https://doi.org/10.3390/bs7030062
6. Sanghamitra P, Eunice L, Sandipana P, et al. Type 2 diabetes and physical activity: barriers and enablers to diabetes control in Eastern India. Prim Health Care Res Dev. 2019;20:e44. doi: https://doi.org/10.1017/S146342361800097X
7. Wu F-L, Tai H-C, Sun J-C. Self-management Experience of Middle-aged and Older Adults With Type 2 Diabetes: A Qualitative Study. Asian Nurs Res (Korean Soc Nurs Sci). 2019;13(3):209-215. doi: https://doi.org/10.1016/j.anr.2019.06.002
8. American Diabetes Association. Improving care and promoting health in populations: Standards of Medical Care in Diabetes – 2019. Diabetes Care. 2019;42(1):S7–S12. doi: https://doi.org/10.2337/dc19-S001
9. Aekplakorn W, Chariyalertsak S, Kessomboon P, Assanangkornchai S, Taneepanichskul S, Putwatana P. Prevalence of Diabetes and Relationship with Socioeconomic Status in the Thai Population: National Health Examination Survey, 2004–2014. J Diabetes Res. 2018;2018:1-8. doi: https://doi.org/10.1155/2018/1654530
10. Clinical Practice Guideline for Diabetes [Internet]. Thai Diabetes Association In the royal patronage of HRH Princess Maha Chakri Sirindhorn. 2017 [cited 2022 Mar 31]. Available from: https://www.dmthai.org/attachments/article/443/guideline-diabetes-care-2017.pdf
11. Reutrakul S, Deerochanawong C. Diabetes in Thailand: Status and Policy. Curr Diab Rep. 2016;16(3):28. doi: https://doi.org/10.1007/s11892-016-0725-7
12. Wichit N, Mnatzaganian G, Courtney M, et al. Randomized controlled trial of a family-oriented self-management program to improve self-efficacy, glycemic control and quality of life among Thai individuals with Type 2 diabetes. Diabetes Res Clin Pract. 2017;123:37-48. doi: https://doi.org/10.1016/j.diabres.2016.11.013
13. Wongrith P. Predicting diabetic self-care management based on the theory of planned behavior among elderly with type 2 diabetes in Thailand. Diabetes Mellit. 2019;22(4):367-376. doi: https://doi.org/10.14341/DM10290
14. Pamungkas RA, Chamroonsawasdi K, Vatanasomboon P, Charupoonphol P. Barriers to Effective Diabetes Mellitus Self-Management (DMSM) Practice for Glycemic Uncontrolled Type 2 Diabetes Mellitus (T2DM): A Socio Cultural Context of Indonesian Communities in West Sulawesi. Eur J Investig Heal Psychol Educ. 2019;10(1):250-261. doi: https://doi.org/10.3390/ejihpe10010020
15. Gupta L, Khandelwal D, Rishi Lal P, et al. Factors Determining the Success of Therapeutic Lifestyle Interventions in Diabetes – Role of Partner and Family Support. Eur Endocrinol. 2019;15(1):18-24. doi: https://doi.org/10.17925/EE.2019.15.1.18
16. Mogre V, Johnson NA, Tzelepis F, Paul C. Barriers to diabetic self‐care: A qualitative study of patients’ and healthcare providers’ perspectives. J Clin Nurs. 2019;28(11-12):2296-2308. doi: https://doi.org/10.1111/jocn.14835
17. Fai EK, Anderson C, Ferreros V. Role of attitudes and intentions in predicting adherence to oral diabetes medications. Endocr Connect. 2017;6(2):63-70. doi: https://doi.org/10.1530/EC-16-0093
18. Oakes AH, Garmo VS, Bone LR, et al. Identifying and Prioritizing the Barriers and Facilitators to the Self-Management of Type 2 Diabetes Mellitus: A Community-Centered Approach. Patient - Patient-Centered Outcomes Res. 2017;10(6):773-783. doi: https://doi.org/10.1007/s40271-017-0248-6
19. Freeman-Hildreth Y, Aron D, Cola PA, Wang Y. Coping with diabetes: Provider attributes that influence type 2 diabetes adherence. PLoS One. 2019;14(4):e0214713. doi: https://doi.org/10.1371/journal.pone.0214713
20. Whittemore R, Vilar-Compte M, De La Cerda S, et al. Challenges to diabetes self-management for adults with type 2 diabetes in low-resource settings in Mexico City: a qualitative descriptive study. Int J Equity Health. 2019;18(1):133. doi: https://doi.org/10.1186/s12939-019-1035-x
About the Authors
P. WongrithТаиланд
Wongrith Paleeratana, RN, NP, M.Sc. (Public Health)
School of Public Health, 222 Walailak University, Tha sala, Nakhon Si Thammarat, 80161
Competing Interests:
Declared no competing interests
P. Thiraratanasunthon
Таиланд
Thiraratanasunthon Phiman, PhD, Assist Prof
Competing Interests:
declared no competing interests
S. Kaewsawat
Таиланд
Kaewsawat Supreecha, PhD, Assist Prof.
Competing Interests:
Declared no competing interests
C. N. Le
Таиланд
Le Cua Ngoc, PhD
Competing Interests:
Declared no competing interests
Supplementary files
|
|
1. Fig. 1. Conceptual Framework. | |
| Subject | ||
| Type | Исследовательские инструменты | |
View
(225KB)
|
Indexing metadata ▾ | |
|
|
2. Неозаглавлен | |
| Subject | ||
| Type | Исследовательские инструменты | |
View
(179KB)
|
Indexing metadata ▾ | |
|
|
3. Неозаглавлен | |
| Subject | ||
| Type | Исследовательские инструменты | |
View
(585KB)
|
Indexing metadata ▾ | |
|
|
4. Fig. 4. Themes in the Patients’ perception and Self-management intention-DSMI. | |
| Subject | ||
| Type | Исследовательские инструменты | |
View
(934KB)
|
Indexing metadata ▾ | |
This is a qualitative study to compare the self-management perceptions of elderly people with diabetes in the glycemic control group and the uncontrollable glycemic group.
The glycemic control group T2DM patients reflected their perceptions and intentions of self-management behavior, which were higher than the uncontrolled group in four themes: reasoning, decision-making, action, and evaluation.
The elderly T2DM patients in the glycemic control group had better family support than those who couldn't control their blood sugar levels
Review
For citations:
Wongrith P., Thiraratanasunthon P., Kaewsawat S., Le C.N. Comparison of Self-Management between Glycemic Controlled and Uncontrolled Type -2 Diabetic Elderly in Thailand: A Qualitative Study. Diabetes mellitus. 2022;25(2):174-185. https://doi.org/10.14341/DM12417
JATS XML

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).















































